Abstract
Abstract 3307
Poster Board III-195
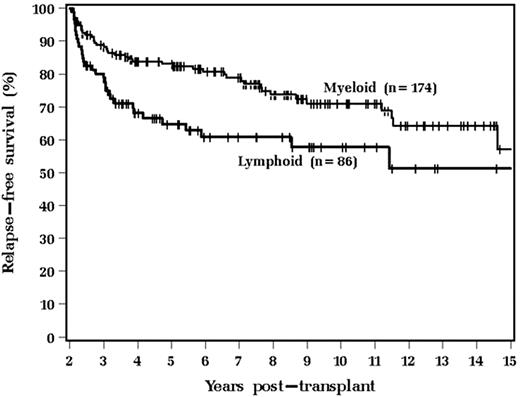
Myeloablative (MA) and reduced-intensity conditioning (RIC) allogeneic hematopoietic stem cell transplantation (alloHSCT) are both effective treatment approaches for patients with otherwise incurable hematologic diseases. However, patients who survive beyond 2 years are still at risk for significant morbidity and mortality. Differences in these later post-transplant outcomes may exist between those patients who received MA and RIC regimens. We therefore investigated outcomes on 677 patients (590 MA and 87 RIC) with hematologic diseases who underwent alloHSCT at our institution from 1/90-12/06. 235 MA and 37 RIC patients survived >2 years (40% vs. 42%, respectively, p=0.63). Factors predictive for surviving >2 years on multivariable analysis included younger age, greater Karnofsky performance status (KPS) at transplant, related donor and HLA matched donor. For > 2 yrs survivors, as compared to those treated with MA conditioning the RIC patients were older (median age 55 vs. 39 yrs, p<0.001), had better KPS at transplant (p<0.001), more commonly had lymphoid diagnoses (24 [65%] vs. 62[28%], p<0.001), had longer median time from diagnosis to transplant (19 vs. 6 mos, p<0.001), had more prior chemotherapy (p<0.001) and radiation therapy (p=0.036), more often received a TBI-based preparative regimen (100% vs. 15%, p<0.001) and peripheral blood stem cells (100% vs. 5%, p<0.001). There were no differences between the groups regarding gender, race, comorbidity index score, donor relationship, donor to recipient gender, HLA matched transplants, incidence or severity of acute or chronic GVHD, CMV infection, other infections or overall survival. Disease relapse was higher in the RIC group (6[16%] vs. 22[9%], p=0.048). Currently, for these >2 yr survivors 178 (76%) MA and 28 (76%) RIC patients remain alive at median follow-ups of 72 (range, 3-196) vs. 33 mos (range, 5-86), respectively (p<0.001). Death occurred most commonly for the MA pts due to relapse, then chronic GVHD, pulmonary toxicity, infection and secondary malignancy, while relapse and secondary malignancy were the most common causes for RIC pts. As compared to those with lymphoid diseases those with myeloid diseases had superior relapse-free survival (RFS) (Figure, p=0.012) and tended to have better overall survival (OS) (p=0.09).
Myeloid disease status was also predictive of lower disease relapse (p=0.005) and better relapse-free survival (p=0.014) on multivariable analysis. However, no differences in CMV infection, other infections, incidence and severity of chronic GVHD, relapse, RFS or OS were found when comparing MA vs. RIC patients for myeloid and lymphoid diseases independently. We conclude that the majority of MA and RIC patients surviving >2yrs after alloHSCT remain alive and relapse-free. The superior RFS for patients with myeloid diseases is likely related to a more robust graft-vs-malignancy effect. Further strategies with novel approaches to decrease late relapses for these patients are warranted.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal