Abstract
Abstract 3183
Poster Board III-120
Over the past 15 years, increased awareness and advances in management such as the widespread adoption of low molecular weight heparins and new anticoagulants have had a dramatic impact on practice; there are no large scale studies to determine the impact of these changes on the health care utilization and outcomes of DVT. We examined national statistics of the trends in hospital utilization for Deep Vein Thrombosis in the United States.
The Nationwide Inpatient Sample (NIS) is one in a family of databases and software tools developed as part of the Healthcare Cost and Utilization Project (HCUP), sponsored by the Agency for Healthcare Research and Quality. For 2007 NIS contains all discharge data from 1,044 hospitals located in 40 States, approximating a 20-percent stratified sample of U.S. community hospitals. We examined trends for hospital utilization available through the NIS dataset. All descriptive statistics have been reported for DVT as ‘primary discharge diagnosis’ as well as ‘All discharge diagnoses’. Presence of ICD-9-CM diagnosis codes 453.0-453.9 were used to define DVT related hospitalizations.
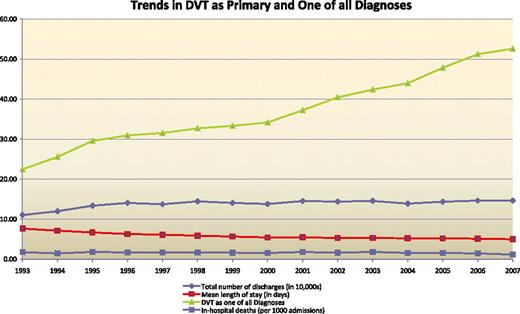
From 1993 to 2007 the number of annual diagnosis of DVT as one of “All Diagnoses' of DVT annually increased from 224,739 to 526,105 while the number of DVT as ‘Principal Diagnosis’ increased from 110,445 to 146,612. The average length of hospital stay has decreased from 7.6 days to 5 days (p-value <0.01). The average annual proportion of in-hospital deaths from DVT decreased during his period from 1.6% vs. 0.8% (p-value <0.01). FIG 1
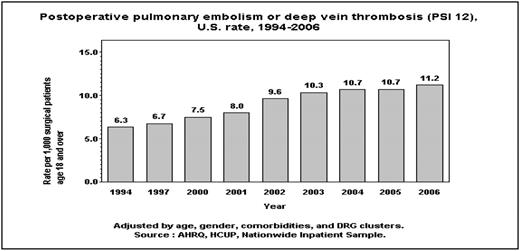
For DVT as one of all diagnoses, the trends show a polynomial upward trend and the rate of increase is increasing every year (p value using T Test: 0.007). For annual number of discharges with DVT as primary diagnosis, there is a polynomial upward trend, with an index less than 1 and the curve is flattening out and the rate of increase is decreasing year over year (p value using T Test=0.0028). These findings suggest that the increase in DVT as primary diagnosis is not keeping pace with rapid increase in DVT as one of all diagnosis. For DVT as primary diagnosis, mortality rate was 1.6% and 0.3% respectively among those who underwent a procedure vs. those who did not undergo a procedure. Mortality for DVT as one of all diagnoses was 8.9% and 3.3% respectively among those who underwent a procedure vs. those did not undergo a procedure. Notably, a death in patients with DVT as one of all diagnosis was attributed to a variety of diagnoses, such as malignancies, infections and complications of implantation device. Rate of postoperative pulmonary embolism or thrombosis per 1000 surgical patients age 18 and over as a marker of Hospital-level Patient Safety Indicators age 18 and over adjusted for age, gender, comorbidities and DRG clusters, has increased from 6.3 in 1994 to 11.2 in 2006 FIG 2.
From 1997 to 2006, the proportion of male patients increased from 43.1% to 45% while female patients decreased from 57% to 54.9%. (p-value <0.01) For the year 2007, with DVT as the primary or one of all diagnoses, OR procedures on vessels other than head and neck is the main principal procedure. DVT of extremities as primary diagnosis is associated with hypertension and hyperlipidemia as most important secondary diagnoses and for all DVT of the extremities as secondary diagnosis the most common primary diagnosis is pulmonary heart disease.
Survival for patients with DVT has improved and patients are likely to be discharged from acute care hospital earlier. We speculate that this could be the result of improved diagnosis and management including the use of low molecular weight heparins. Some of the changes in annual incidence may be attributed to earlier diagnosis and changes in ICD coding. However, the sustained increase in annual incidences of DVT as a secondary diagnosis and that of postoperative pulmonary embolism and thrombosis is a cause for concern and should prompt a review of strategies to prevent DVT among sick hospitalized patients. These data are subject to the well known limitations of administrative datasets, and underscore the need for large scale prospective study of the factors contributing to health care utilization and outcomes of DVT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal