Abstract 2978
Poster Board II-949
Post-thrombotic syndrome (PTS) is a condition of chronic venous insufficiency following deep venous thrombosis (DVT) that affects both adults and children. Nevertheless, investigation of PTS in children has lagged behind that in adults.
This systematic review was undertaken to summarize evidence from the pediatric literature on the prevalence of PTS, the validity of proposed measures of PTS, and prognostic factors for PTS in children.
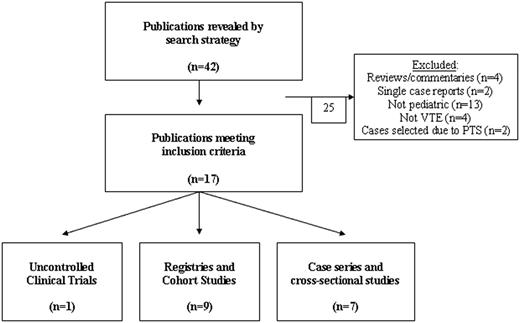
A comprehensive Medline search was performed employing the following terms: “[pediatric OR children] AND [post-thrombotic syndrome OR post-phlebitic syndrome]”. Single case reports, narrative reviews, and commentaries were excluded.
Seven case series and cross-sectional studies, nine registries and cohort studies, and one uncontrolled clinical trial were identified that met inclusion criteria; these studies reported on a total of 1316 children with DVT (Table 1). The prevalence of PTS differed substantially between observational and non-observational studies: 15% of 1042 children versus 46% of 274 children, respectively. No pediatric studies have evaluated quality of life (QOL) associated with PTS. Two reports from a single-institutional cohort have identified elevated levels of factor VIII and D-dimer and non-use of thrombolytic therapies as potentially prognostic of PTS in children, particularly among those with veno-occlusive thrombi; these are the only reports employing a PTS outcome measure that has been validated in children (the Manco-Johnson instrument).
Results of comprehensive Medline search strategy for original reports on pediatric PTS (see also Methods), including data on PTS prevalence among children with venous thrombosis.

Overall, high-quality evidence on pediatric PTS is lacking. Collaborative prospective cohort studies and trials that use validated measures of pediatric PTS are needed to assess the incidence of, prognostic factors for, and QOL impact of PTS in children.
No relevant conflicts of interest to declare.
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal