Abstract
Abstract 2697
Primary testicular lymphoma (PTL) is the most common testicular neoplasm in males over the age of 60, representing 1% to 7% of all testicular malignancies. Histologically, the most common subtype of PTL is diffuse large B-cell lymphoma (DLBCL) representing 80–90% of diagnosed tumors. Primary testicular lymphoma has a tendency to disseminate to the contralateral testis and the central nervous system. Treatment approaches can include loco-regional treatment regimens (orchiectomy, radiotherapy) and systemic chemotherapy with or without intra-thecal chemoprophylaxis. The purpose of this study is to determine the clinical characteristics, patterns of failure, and survival of patients with PTL at our institution and to determine any correlation between outcome and treatment strategies.
We retrospectively reviewed the medical records of patients with diffuse large B cell lymphoma of the testis. All patients were diagnosed and managed at the University of Texas MD Anderson Cancer Center between 1964 and 2008. Pathological diagnosis of DLBCL of the testis was made from orchiectomy specimens or fine needle aspiration of the testis. Factors analyzed included: age, stage at diagnosis, presence of b-symptoms, serum lactate dehydrogenase (LDH), beta-2 microglobulin, and modality of treatment. Cox proportional hazards model was used to generate hazard ratios for prognostic factors that affect the overall survival (OS) and disease free survival (DFS). Estimates of survival were calculated using the Kaplan-Meier method and the log-rank test was used to compare OS and DFS by the type of treatment.
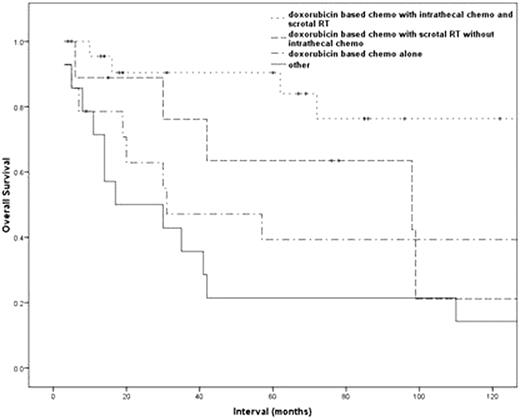
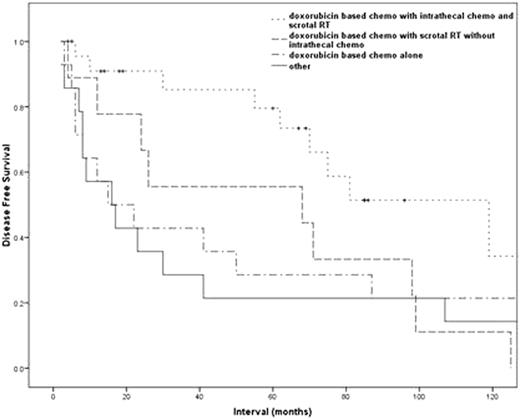
Seventy-five patients with DLBCL of the testis were identified. The median age at diagnosis was 64 years (range 22 – 82). Ann Arbor stage I was present in 34 (45%), stage II in 13 (17%), stage III in 4 (5%), stage IV in 23 (31%), and unknown in 1 (1%). On univariate analysis, patients with advanced stage disease (stage III and IV; p = 0.042), elevated serum LDH levels (p = 0.029), B-symptoms at presentation (p = 0.003), and high-intermediate and high IPI score (p = 0.013), had a significantly decreased OS and DFS. The 5-years OS and DFS for all patients was 53.3%, and 45.9%, respectively. Treatment details are described in Table 1. A greater proportion of patients who received trimodality regimen (doxorubicin based chemotherapy, scrotal RT, and intrathecal methotrexate) had limited stage disease compared to those receiving less than a trimodality approach, however this variation was not statistically significant (71% vs 60%; p = 0.374, chi-square test). The 5-year OS and DFS for those treated with trimodality regimen was 90.4% and 79.5%, respectively, while for those treated with doxorubicin-based chemotherapy and testicular irradiation but without intrathecal chemotherapy it was 63.5%, and 55.6%, respectively, and for those treated with doxorubicin-based chemotherapy alone it was 39.3%, and 28.6% (p = 0.009 for OS and p = 0.012 for DFS). Figures 1 & 2
Summary of treatment regimen excluding surgical resection.
| Type of Treatment . | No. of Patients . | % . |
|---|---|---|
| Doxorubicin based chemo with intrathecal chemo and scrotal RT | 24 | 32 |
| Doxorubicin based chemo with scrotal RT without intrathecal chemo | 9 | 12 |
| Doxorubicin based chemo with intrathecal chemo without scrotal RT | 7 | 9 |
| Doxorubicin based chemo alone | 14 | 19 |
| Other | 15 | 20 |
| Unknown | 6 | 8 |
| Type of Treatment . | No. of Patients . | % . |
|---|---|---|
| Doxorubicin based chemo with intrathecal chemo and scrotal RT | 24 | 32 |
| Doxorubicin based chemo with scrotal RT without intrathecal chemo | 9 | 12 |
| Doxorubicin based chemo with intrathecal chemo without scrotal RT | 7 | 9 |
| Doxorubicin based chemo alone | 14 | 19 |
| Other | 15 | 20 |
| Unknown | 6 | 8 |
Prognostic factors for DLBCL of the testis include stage, LDH, B-symptoms, and IPI score. Patients with DLBCL of the testis who received trimodality regimen (doxorubicin based chemotherapy combined with scrotal RT and intrathecal chemotherapy) had significantly improved OS and DFS, which support the use of this approach as standard of care.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal