Abstract
Poster Board II-587
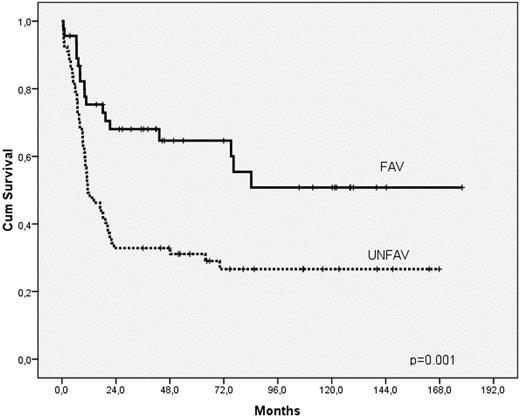
The prognostic heterogeneity of patients with intermediate-risk cytogenetics AML (AML-IR) is mostly clarified by determination of mutations of NPM1 gene (NPMmut) and internal-tandem duplication of FLT3 gene (FLT3-ITD). Nonetheless, other genetic lesions described in this population might contribute to a better prognostic categorization. In this context, we analyzed the presence of CEBPA mutations and associated features in patients with AML-IR lacking both NPMmut and FLT3-ITD. Overall, 136 patients (51% female; median age: 53, range: 17=74) diagnosed with de novo AML-IR (MRC definition) in our institution between 1994 and 2008 who received standard AML chemotherapy were included in the analysis. CEBPA mutations (CEBPAmut) were investigated by whole gene sequencing using 4 primer pairs according to previously reported methods (Fröhling et al, 2004). Sixty-five patients (48%) harbored NPM1 mutations, 30 of them having concomitant FLT3-ITD. Among NPM1 wild-type patients (NPMwt), FLT3-ITD, CEBPA and MLL mutations were detected in 18, 11, and 5 patients, respectively. Regarding cases with CEBPAmut, biallelic mutations were found in 8 patients, including 6 cases with combined mutations of N-terminal and bZIP domains and two homozygous mutations, whereas a single mutation in bZIP domain was found in the three remaining patients. As compared to patients with wild-type CEBPA (CEBPAwt), those with CEBPAmut were younger (29 vs. 53, p=0.027), and showed a trend to male predominance (73 vs. 46%, p=0.09) and lower WBC count at presentation (16 vs. 33.5 × 109/L, p=.095). Of note, CD7 antigen was aberrantly expressed in virtually all CEBPAmut cases (10/11), compared to only 21% of CEBPAwt patients (p<0.001). Moreover, an abnormal karyotype was observed in 4 patients with CEBPAmut. In the overall series, complete response rate (CR), survival (OS), and relapse incidence (RI) were 83%, 39±4% (5-yr), and 50±5% (5-yr), respectively. Independent favorable factors for survival were younger age (<median; RR: 1.9, 95% CI: 1.2-3, p=0.004), low WBC count at diagnosis (< median; RR: 1.7, 95% CI: 1.1–2.6, p=0.025) and NPMmut/FLT3-ITDneg status (RR: 2.4, 95% CI: 1.3–4.2, p=0.003). Remarkably, patients with CEBPAmut showed a favorable outcome, with a trend for a more prolonged survival, compared to patients with a high-risk NPM/FLT3 status (5-year OS in pts <60 years: 74±16% vs. 33±6%, p=0.087). Based on these results, patients were grouped in a favorable (i.e., either NPMmut /FLT3-ITDneg or CEBPAmut, FAV) or unfavorable molecular category (i.e., those with FLT3-ITD, double NPMwt and CEBPAwt configuration, or MLL abnormalities, UNFAV); these two groups had independent prognostic impact on OS (RR: 2.3, 95% CI: 1.3–4, p=0.001; see figure), RI (RR: 2.2, 95% CI: 1.2–4.3, p=0.016), and leukemia-free survival (RR: 2.2, 95% CI: 1.3–3.7, p=0.002). Importantly, the outcome of patients in the FAV group did not differ according to post-remission treatment (autologous vs. allogeneic stem-cell transplantation, SCT), whereas relapse risk was significantly higher in patients with unfavorable markers who received autologous SCT (60±13% vs. 18±12%, p=0.03). In summary, the assessment of CEBPA mutations, especially in patients lacking NPMmut and FLT3-ITD and expressing CD7 antigen, may refine the molecular prediction of prognosis and guide therapeutic strategy in patients with intermediate-risk AML.
Legend for figure. Survival of patients with intermediate-risk cytogenetics AML according to molecular risk
Legend for figure. Survival of patients with intermediate-risk cytogenetics AML according to molecular risk
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal