Abstract
Abstract 2313
Poster Board II-290
The ability to receive an autologous stem cell transplant (ASCT) is the main factor determining outcome in patients with refractory or relapsed aggressive non-Hodgkin lymphoma (NHL). Final eligibility for ASCT is mainly dependent on response to salvage therapy. The secondary age-adjusted international prognostic index (saa-IPI) at relapse can predict for response to salvage therapy and outcome after transplantation. In allogeneic settings, comorbidity according to the stem cell transplant comorbidity index (HCT-CI) has shown to be an independent predictor for survival in hematologic malignancies. The aim of the current analysis is to assess the additional prognostic value of comorbidity at time of relapse (R-HCT-CI) for ASCT eligibility and outcome after autologous transplant.
We retrospectively analyzed 156 consecutive patients with refractory or relapsed NHL, referred to our center for salvage chemo-immunotherapy between 1999 and 2007. Patients responding to salvage treatment and able to receive further treatment were considered eligible for subsequent high-dose chemotherapy and ASCT. Comorbidity according to the hematopoietic stem cell transplant comorbidity index (Sorror et al; Blood 2005) was scored twice: i at relapse (R-HCT-CI), before start of salvage re-induction and ii. at start of high-dose chemotherapy (BEAM) before ASCT (HCT-CI). Primary endpoints were receipt of actual transplantation and overall survival (OS).
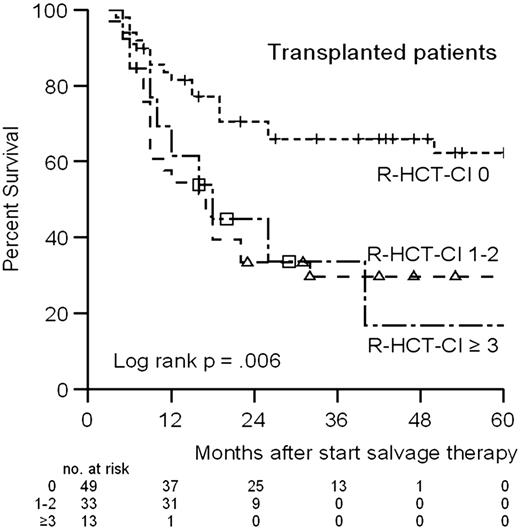
R-HCT-CI scores of 0, 1-2 and ≥3 were found among 64 (41%), 62 (40%) and 30 (19%) patients, respectively at relapse. Comorbidity at transplantation (HCT-CI) did not substantially differ from scores at time of relapse. 108/156 patients achieved at least PR after salvage chemo-immunotherapy. All responsive patients were considered eligible to receive ASCT. Of these responsive patients, 13 did not receive ASCT mainly because of progressive lymphoma just before starting BEAM. Ultimately 95 patients received ASCT. Higher R-HCT-CI scores were associated with significant less chance on receiving ASCT with odds ratios of 2.9 and 4.3 for R-HCT-CI scores of 1-2 and ≥3 respectively (p< .01). However, in multivariate analysis together with saa-IPI scores, comorbidity did not retain significance (p= .08). Comorbidity at relapse could predict for overall survival independent from saa-IPI scores: hazard ratios of 2.5 and 1.7 for R-HCT-CI scores of 1-2 and ≥3 respectively (p= .02). Overall survival rates at 5 years for transplanted patients were 62%, 30% and 17% for R-HCT-CI scores of 0, 1-2 and ≥3 respectively (Figure).
In patients with relapsed aggressive NHL, comorbidity at relapse can predict for ASCT eligibility and, after transplantation, for subsequent survival independently from saa-IPI. Both indices can therefore contribute to a more accurate selection of patients who may benefit most from intensive salvage treatment and subsequent ASCT.
Overall survival according to Comorbidity score at relapse for patients receiving ASCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal