Abstract
Abstract 2296
Poster Board II-273
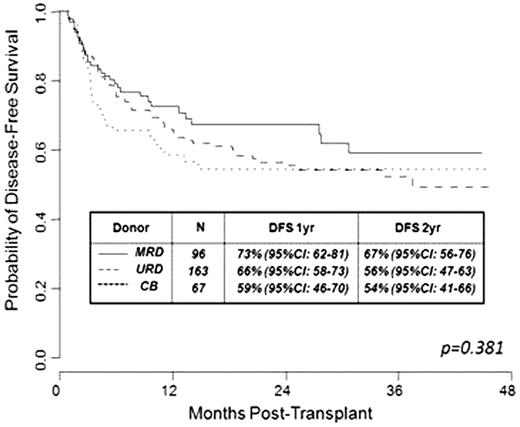
CB transplantation (CB-T) may be curative for patients with high-risk or advanced hematologic malignancies. However, given there are no randomized trials comparing survival after CBT with the more traditional approach of matched related donor transplantation (MRD-T) or unrelated donor transplantation (URD-T), how CB-T compares to MRD-T and URD-T transplantation is not established. Therefore, we conducted a retrospective study comparing survival after CB-T (n=67) with MRD-T (n=96) and URD-T (n=163) performed 10/05-3/09 for the treatment of hematologic malignancies. Our hypothesis was that 1 year survival is comparable between hematopoietic stem cell (HSC) sources. Consecutive adult and pediatric recipients of first allograft for the treatment of acute leukemia in remission (CR1-3), myelodysplasia (MDS, ≤5% blasts at work-up), or non-Hodgkins or Hodgkin lymphoma were eligible for analysis. The median age of CB-T recipients (37 years, range <1-66) was not different to that of MRD-T (46 years, range <1-71) and URD-T (47 years, range 1-71) recipients (p=0.151). A lower percentage of CB-T recipients (n=36, 54%) had acute leukemia or MDS as compared to 69 (72%) MRD-T and 116 (71%) URD-T recipients (p=0.022), and a lower percentage received ablative conditioning (n=47, 70%) as compared to 81 (84%) MRD-T and 141 (87%) URD-T recipients (p<0.001). While MRD grafts were HLA-identical, URD grafts were 8-10/10 HLA-allele matched (99 10/10, 47 9/10, 17 8/10). CB grafts were 4-6/6 HLA-A,-B antigen, DRB1 allele matched, with all CBT recipients receiving double unit grafts (median infused TNC larger unit 2.57 × 107/kg; smaller unit 1.93 × 107/kg) to augment engraftment. GVHD prophylaxis was calcineurin inhibitor based in 67 (100%) of CB-T but only 37 (39%) of MRD-T and 52 (32%) of URD-T recipients, with remaining patients receiving T cell depleted grafts. Median follow-up of survivors is 22 months (range 5-46) and was similar between HSC sources. We found no difference in the cumulative incidence (CI) of transplant-related mortality (TRM) at day 100 between HSC sources: 15% (95%CI: 6-24) in CB-T as compared to 7% (95%CI: 2-13) for MRD-T and 10% (95%CI: 5-14) for URD-T recipients (p=0.742). Further, there was no difference in the CI of relapse at 1 year: 19% (95%CI: 9-29) in CB-T as compared to 16% (95%CI: 9-24) for MRD-T and 16% (95%CI: 10-22) for URD-T recipients (p=0.930). Finally, by log-rank analysis there was no significant difference between HSC sources for either overall survival (p=0.778) or disease-free survival (DFS, p=0.381, Figure 1). While outcomes within subgroups could differ according to HSC source as well as donor-recipient HLA-match, recipient co-morbidities, diagnosis, disease risk, conditioning intensity, and GVHD prophylaxis, this encouraging preliminary data supports the use of double unit CB grafts as an alternative HSC source in patients lacking suitably HLA-matched peripheral blood HSC or marrow donors.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal