Abstract
Abstract 1780
Poster Board I-806
Myelodysplastic syndromes (MDS) in pediatrics comprise a heterogenous group of disorders that are poorly understood and difficult to treat. Allogeneic HPCT remains the only curative treatment, but published outcomes in children are limited.
We performed a retrospective review of pediatric patients with MDS who received an allogeneic HPCT on IRB approved protocols between 1992 and 2009 at Children's Memorial Hospital (Chicago, IL).
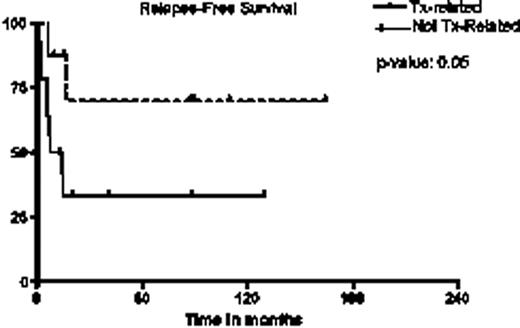
The study population consisted of 23 consecutive patients. Median age at transplant was 9.2 years (range 4.6-17.2 years) and median time to transplant from diagnosis was 4.3 months (range 2.2-9.9 months). Nine patients (39%) had de novo MDS, whereas 14 of 23 (61%) patients had treatment-related MDS, and 4 patients in this group had received a previous autologous transplant for a previous malignancy. All patients had a documented cytogenetic abnormality: monosomy 7/7q- in 12 patients (52%), trisomy 8 in 3 (13%), translocation (6;9) in 3 (13%), and others in 5 (22%). Donors were HLA matched siblings in 8 cases (35%), 8/8 loci HLA matched unrelated donors in 6 (26%), and the remaining 9 (39%) were 6-7/8 loci HLA mismatched unrelated donors. HPC source was peripheral blood in 13 patients (57%), cord blood in 7 (30%), and bone marrow in 3 (13%). Fourteen of 23 (61%) patients received a myeloablative conditioning regimen with TBI/Cy in 9 (31%), Bu/Cy in 4 (17%), and Flu/Bu/low-dose TBI in 1. Reduced intensity conditioning (RIC) regimens were used for the remaining 9 (39%) and consisted of Flu/Bu/ATG. Indications for RIC transplant included patient choice in 4 patients, prior autologous transplants in 3 patients, and comorbid conditions in 2 patients. Twenty patients (90%) had evidence of engraftment, with only 1 death prior to day 100. Seven patients (30%) died secondary to transplant-related complications, including infection in 4, GVHD in 2, and toxic epidermolysis in 1. Of the 4 patients that had received a prior transplant, 3 died from transplant-related mortality. Grade 2-4 acute and chronic graft-versus-host disease (GVHD) was seen in 9 (39%) and 11 (48%) patients, respectively. For the entire group, estimated five year relapse-free survival (RFS) and overall survivals (OS) were 47% [95% CI: 28%, 67%] and 50% [95% CI: 25.1%, 71.1%], respectively. Two patients had graft failure, which included 1 patient who received cord blood and 1 patient who received peripheral blood with RIC. Five patients suffered a relapse of original disease, including 3 patients who received RIC. These 3 patients each received a second myeloablative transplant; 2 of these patients remain alive and disease-free. Treatment-related MDS was associated with decreased RFS in comparison to non-treatment-related MDS (33% [95% CI: 11%, 58%]) vs. 70% [95% CI: 22%, 92%], p=0.05). In contrast, five year OS rates reached 80% for those with de novo MDS. There was no significant difference in overall survival between patients who received RIC versus myeloablative conditioning (p=0.17), but RIC regimens were associated with decreased relapse-free survival in comparison to myeloablative conditioning regimens (22% [95% CI: 3%, 51%] vs. 68% [95% CI: 34%, 87%], p=0.02). On univariate analysis, there was no correlation of relapse-free or overall survival with blast count at diagnosis, IPSS score, type of cytogenetic abnormality, receiving AML-like chemotherapy for MDS, CMV serostatus, donor type and HLA match, cell dose, and time to transplant.
Allogeneic HPCT is a curative option for pediatric MDS. In this series of high risk patients we achieved OS approaching 80% in patients with de novo MDS. Those who received RIC had an increased relapse rate but were salvaged by myeloablative conditioning regimens and had comparable outcomes to the myeloablative group. The role of RIC regimen transplants in pediatric MDS needs to be studied further. Larger series of pediatric patients are needed to establish a prognostic scoring system to predict outcome and select appropriate conditioning regimens to further improve survival in allogeneic HPCT for MDS.
Treatment-related vs. Non-treatment related MDS
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal