Abstract
Abstract 1624
Poster Board I-650
Activating type I mutations provide cells with proliferative and survival advantages. Together with type II abnormalities, which cause a differentiation arrest and an increase in self-renewal properties, they cooperate to cause acute myeloid leukemia (AML). Currently, many novel drugs have been developed to specifically target these mutations and the mutations are also used as marker of malignant cells in MRD detection. It is thus of importance to accurately determine the mutation status of AML samples. Our previous study showed frequent shifts in FLT3/ITD mutations between initial and relapse samples. Losing an FLT3/ITD mutation at relapse was associated with prolonged time to relapse, whereas acquiring an FLT3/ITD at relapse was associated with a shorter time to relapse (Cloos et al. Leukemia, 2006). We now extended the mutation analysis of paired initial and relapsed pediatric samples to study the stability of type I and II mutations including RAS oncogenes (e.g. N-RAS, K-RAS), receptor tyrosine kinases (FLT3 and KIT), WT1, NPM1, PTPN11 and CEBPá genes.
Samples were analyzed of 70 pediatric AML patients who were treated with protocols of the BFM-AML Study Group or Dutch Childhood Oncology Group between 1992 and 2004. Using capillary gel electrophoresis based fragment analysis, we analyzed the patient samples for insertions/deletions in exons 14, 15 and 20 of FLT3, exon 11 of KIT, exon 12 of NPM1 and 3 hotspots in the CEBPá gene. FRET based melting curve analysis or high resolution melting curve analysis were used to detect point mutations in exons 8, 9 and 17 of KIT, exons 3 and 13 of PTPN11, codon 12/13 and 61 mutations of N-RAS and codon 12/13 mutations of K-RAS. Exons 7,8,9 and 10 of WT1 were screened using multiplex ligation probe amplification.
Instabilities were found in 25 out of 70 (36%) patients (Table 1). In none of the cases a mutation at diagnosis predicted time to relapse. However, when patients were stratified according to the presence of a type I/II mutation at relapse, independent of its presence at diagnosis, patients who had a FLT3/ITD or RAS mutation at relapse, experienced a significantly shorter mean time to relapse than patients without a mutation at relapse (Table 2).
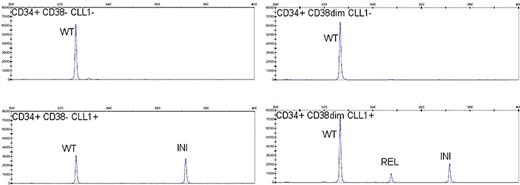
One possible explanation for the observed shifts in type I/II aberrations is the expansion at relapse of minor leukemic sub-clones, present, but not detected at diagnosis. Of a patient of whom we had enough cryopreserved cells from diagnosis samples available to FACSsort small amounts of cells (<25) from different primitive leukemic blast compartments. We found that the malignant progenitor like CD133-CD34+CD38dim fraction contained a clone with the type I/II molecular profile which was present at relapse but was not detected in the bulk of the diagnosis sample (Figure 1).
In conclusion, in a relatively large cohort of paired diagnosis-relapse samples, we established that a high percentage (nearly 40%) of pediatric AML patients show changes in type I/II mutations, with both gains and losses from diagnosis to relapse. This indicates that mutation profiling at diagnosis is often not sufficient for accurate relapse risk assessment. Additional molecular characterization of AML at minimal residual disease will guide targeted therapy. The mutational shifts can be explained by the expansion of minor leukemic sub-clones during evolution of the disease. Although we show clonal selection in one case we cannot rule out the possibility that in other patients the observed shifts are due to the development of new leukemic sub-clones which are induced during therapy and related to genomic instability. To elucidate this, future research will focus on the detection and characterization of malignant sub-clones at different stages of the disease.
Financially supported by Dutch Cancer Society (VU 2005-3666)
Frequency of mutation shifts in genes of interest for 70 paired pediatric AML samples
| Gene of interest . | FLT3/ITD . | FLT3 D835 . | RAS . | WT1 . | KIT . | PTPN11 . | NPM1 . | CEBPá . |
|---|---|---|---|---|---|---|---|---|
| Gain | 2 | 1 | 4 | 5 | 0 | 0 | 0 | 1 |
| Loss | 4 | 1 | 7 | 0 | 0 | 1 | 1 | 0 |
| Gene of interest . | FLT3/ITD . | FLT3 D835 . | RAS . | WT1 . | KIT . | PTPN11 . | NPM1 . | CEBPá . |
|---|---|---|---|---|---|---|---|---|
| Gain | 2 | 1 | 4 | 5 | 0 | 0 | 0 | 1 |
| Loss | 4 | 1 | 7 | 0 | 0 | 1 | 1 | 0 |
Association between mean time to relapse and mutation status
| . | time of analysis . | mean time to relapse (months, neg vs. pos) . | ANOVA p value . |
|---|---|---|---|
| FLT3/ITD | diagnosis | 16.0 vs 17.2 | 0.8 |
| relapse | 17.8 vs 7.8 | 0.05 | |
| RAS | diagnosis | 18.0 vs 11.2 | 0.1 |
| relapse | 18.4 vs 9.4 | 0.01 | |
| WT1 | diagnosis | 17.5 vs 15.1 | 0.7 |
| relapse | 18.6 vs 12.5 | 0.28 |
| . | time of analysis . | mean time to relapse (months, neg vs. pos) . | ANOVA p value . |
|---|---|---|---|
| FLT3/ITD | diagnosis | 16.0 vs 17.2 | 0.8 |
| relapse | 17.8 vs 7.8 | 0.05 | |
| RAS | diagnosis | 18.0 vs 11.2 | 0.1 |
| relapse | 18.4 vs 9.4 | 0.01 | |
| WT1 | diagnosis | 17.5 vs 15.1 | 0.7 |
| relapse | 18.6 vs 12.5 | 0.28 |
SEQ Figure \* ARABIC 1: FLT3/ITD analyis on cell sorted fractions from a diagnosis sample. Abbreviations; WT=wild type, INI=initial ITD, REL=relapse ITD
SEQ Figure \* ARABIC 1: FLT3/ITD analyis on cell sorted fractions from a diagnosis sample. Abbreviations; WT=wild type, INI=initial ITD, REL=relapse ITD
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal