Abstract
Abstract 1374
Poster Board I-396
Allogeneic stem cell transplantation is the only potentially curative therapeutic option for patients with CLL. However, in spite of recent improvements in transplant-related mortality due to the introduction of reduced-intensity conditioning (RIC), only a proportion of patients go on to receive a stem cell transplant. The aim of this study was to quantify how many patients are evaluated for transplant versus how many go on to transplant, and to examine the reasons why transplantation was not performed.
A list of all patients with CLL who have been referred to the Ohio State University for a transplant evaluation from January 2003 to the present was obtained. Two electronic databases, E-Results and TransChart, were reviewed to determine if a consultation was performed, if patients were subsequently transplanted, and if not, why.
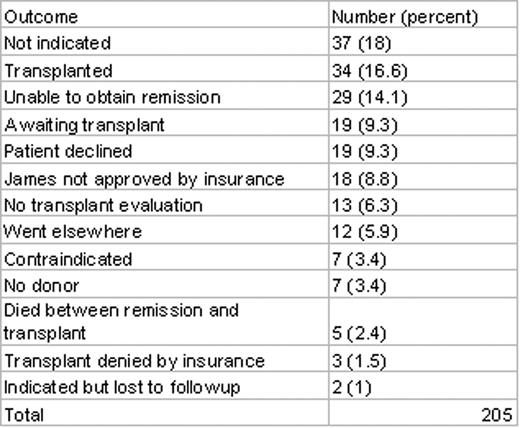
The outcomes of the referrals are summarized in Table 1. From January 2003 to the present, 205 patients with CLL were referred to our center for a transplant evaluation. Of those, 34 (16.6%) underwent transplantation. For patients who did not receive a transplant, it was not indicated at the time of consult according to current standard of care in 37 patients (18%), and in 29 (14.1%), transplant was indicated but patients were unable to obtain a remission in order to proceed. The differences between patients who went on to transplant and those who could not obtain remission were analyzed more closely. The median age in the transplant group was 55, and the median age in the group that could not obtain remission was 58. Both groups received a median 2 lines of treatment prior to transplant evaluation. The cytogenetic abnormalities of the groups are summarized in Table 2.
The majority of patients who did not undergo transplantation did not have an indication for transplant, reflecting previous standards of care prior to the understanding of the poor prognosis of patients with high risk karyotype and fludarabine-refractory CLL. In contradistinction, an inability to obtain a remission in order to proceed to transplantation was the second most common reason transplantation was deferred. These data reflect the difficulty in some cases of determining the appropriate timing for allogeneic transplantation in CLL and the risk of delaying a transplant referral in patients with fludarabine refractory disease. Appropriate timing of transplant referral and choice of effective salvage therapy are critical to the successful long-term management of patients with fludarabine-refractory CLL.
| Cytogenetic abnormality . | Transplanted . | No remission . | p value . |
|---|---|---|---|
| del17p | 11 | 15 | 0.0968 |
| del11q | 3 | 2 | 0.577 |
| del13q | 2 | 4 | 0.263 |
| trisomy 12 | 2 | 0 | 0.287 |
| del11q and 13q | 4 | 3 | 0.591 |
| del17p and 11q | 2 | 0 | 0.287 |
| del17p and 13q | 3 | 0 | 0.151 |
| del6q | 1 | 0 | 0.54 |
| t(14;19) | 3 | 1 | 0.369 |
| normal | 3 | 2 | 0.577 |
| unknown | 0 | 2 | 0.208 |
| Total | 34 | 29 |
| Cytogenetic abnormality . | Transplanted . | No remission . | p value . |
|---|---|---|---|
| del17p | 11 | 15 | 0.0968 |
| del11q | 3 | 2 | 0.577 |
| del13q | 2 | 4 | 0.263 |
| trisomy 12 | 2 | 0 | 0.287 |
| del11q and 13q | 4 | 3 | 0.591 |
| del17p and 11q | 2 | 0 | 0.287 |
| del17p and 13q | 3 | 0 | 0.151 |
| del6q | 1 | 0 | 0.54 |
| t(14;19) | 3 | 1 | 0.369 |
| normal | 3 | 2 | 0.577 |
| unknown | 0 | 2 | 0.208 |
| Total | 34 | 29 |
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal