Abstract
Higher prevalence of asymptomatic or benign neutropenia has been observed in individuals of African descent compared to Caucasians and Hispanics. Although this condition is presumed to be benign, there has been no study directly examining its effects on overall survival. Our study was conducted to better understand the predictive value of absolute neutrophil counts (ANCs) on survival among outpatients of different ethnicities in a large inner city elderly cohort.
A total of 35,887 individuals 65 years of age and older seen at Montefiore medical system outpatient clinics from January 1st 1997 to May 1st 2008 who underwent a complete blood count within 3 months of the visit were included in the cohort. Using the generally accepted definition of an ANC <1500/microL, we determined 0.6% of Caucasians (out of 8,780), 2.8% of African Americans (out of 9,483), and 1.4% of Hispanics (out of 11,639) were neutropenic at baseline (p<0.001 for both comparisons with Caucasians). The higher prevalence of neutropenia in African Americans and Hispanics was maintained even after excluding patients with baseline anemia and thrombocytopenia (Caucasians 0.2%, African Americans 2.0%, Hispanics 1.0%; p<0.001 for both comparisons).
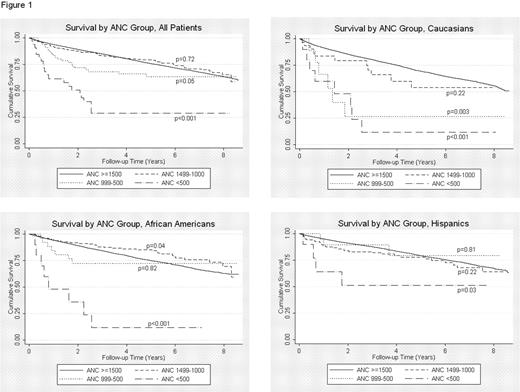
We further categorized neutropenia as “mild” for ANCs between 1499 to 1000/microL, “moderate” for ANCs between 999 to 500/microL, and “severe” for ANCs <500/microL. The increased prevalence of neutropenia noticed in African American and Hispanic populations was mainly found to be restricted to the “mild” subgroup only. Age-adjusted Hazard Ratios (HRs) using ANC ≥1500/microL as reference did not demonstrate increased overall mortality in patients with “mild” neutropenia in any ethnic group. “Moderate” neutropenia, however, was associated with increased mortality in Caucasians (HR=2.9, p=0.01) but not in African Americans (HR=1.1, p=0.72) or Hispanics (HR=1.0, p=0.99). Patients with “severe” neutropenia had significantly increased overall mortality regardless of ethnicity (Caucasians HR=5.1, p<0.001; African Americans HR=8.5, p<0.001; Hispanics HR=3.0, p=0.03). Kaplan-Meier curves by different levels of neutropenia and ethnicity are presented in Figure 1.
We also categorized differing total white blood cell (WBC) counts as “mild” leukopenia (4700 to 4000/microL) or “moderate” leukopenia (<4000/microL) and calculated age-adjusted HRs using a WBC range of 4800 to 10800/microL as reference. “Mild” leukopenia was not associated with increased mortality in all ethnic groups (Caucasians HR=0.9, p=0.35; African Americans HR=0.8, p=0.01; Hispanics HR=0.9, p=0.29), but “moderate” leukopenia was associated with increased mortality in both Caucasians (HR=1.8, p<0.001) and Hispanics (HR=1.5, p<0.001), but not in African Americans (HR=1.0, p=0.88).
In conclusion, we confirmed a higher prevalence of mild neutropenia in African Americans and Hispanics compared to Caucasians in a large elderly outpatient cohort. An ANC <500/microL is mostly associated with other cytopenias, is likely secondary to bone marrow suppression or dysfunction and consequently is associated with decreased survival across all ethnicities. Clinically, an ANC <1000/microL is associated with increased mortality in Caucasians but not in African Americans and Hispanics. For the latter groups, only an ANC <500/microL resulted in decreased survival. A total WBC <4000/microL is associated with increased mortality in Caucasians and Hispanics, but not in African Americans. Our results suggest that the functional capacity of neutrophils may differ by ethnicity and that definitions for clinically relevant neutropenia may require different cutoffs based on ethnicity.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal