Abstract
Abstract 1149
Poster Board I-171
Nonmyeloablative conditioning followed by allogeneic hematopoietic cell transplantation (HCT) has been increasingly used as treatment for elderly patients with hematologic malignancies. It has been suspected that T cell reconstitution would be impaired in elderly patients given nonmyeloablative conditioning because of age-related thymic atrophy. Here, we investigated long term lymphocyte reconstitution and thymic function in 80 patients given allogeneic peripheral blood stem cells (PBSC) after nonmyeloablative conditioning.
Median age at transplant was 57 years (range 10-71). Conditioning regimen consisted of 2 Gy total body irradiation (TBI) with (n=46) or without (n=20) added fludarabine, 4 Gy TBI with fludarabine (n=6), or cyclophosphamide plus fludarabine (n=8). Thirty-three of the 80 patients received grafts from HLA-matched related donors, 22 from HLA-matched unrelated donors, and 25 from HLA-mismatched related or unrelated donors. PBSC were unmanipulated in 56 patients, CD8-depleted in 19 others, and CD34-selected in the remaining 5 patients. GVHD prophylaxis consisted of mycophenolate mofetil and cyclosporine or tacrolimus. Immune recovery was assessed between 1 and 8.5 years after HCT by signal-joint T-cell receptor excision circle (sjTREC) quantification (221 samples), and flow cytometry. Further, in order to demonstrate a potential thymic recovery, sjTREC level changes from day 100 to days 365 and 730 were also assessed by using Wilcoxon signed rank tests.
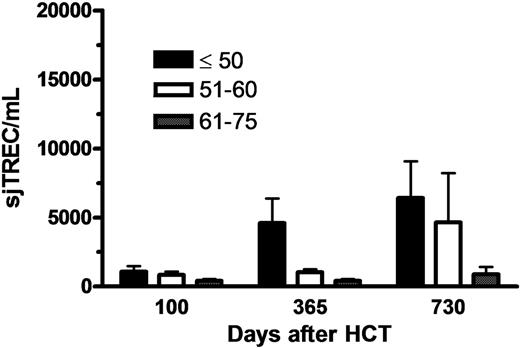
There was a close correlation between sjTREC levels and naive CD4+ T cells (defined as CD4+CD45RA+) counts (P<0.0001). An inverse correlation was observed between the levels of sjTREC/ml and the recipient's age (R=-0.41, p<0.0001). Interestingly, sjTREC levels increased from day 100 to 1 and 2 years after transplantation in patients ≤ 50 (n=23; P=0.02 and P=0.04, respectively), and in those 51-60 years of age (n=35; P=0.17 and P=0.06, respectively), but not in patients >60 (n=22; P=0.3 and P=0.3, respectively) (Figure 1). Similarly, naïve CD4 T cell counts increased from day 100 to 1 and 2 years after transplantation in patients ≤50 (n=23; P=0.01 and P=0.3, respectively), and in those 51-60 years of age (n=35; P=0.5 and P<0.001, respectively), but not in patients >60 (n=22; P=0.9 and P=1.0, respectively). In multivariate analyses, older patient age (P<0.001), extensive chronic GVHD (P<0.001), and prior (resolved) extensive chronic GVHD (P=0.008) were associated with low sjTREC levels, while older patient age (P<0.001), and extensive chronic GVHD (P<0.001) were associated with low naïve CD4 T cell counts.
Our data suggest that thymic neo-generation of T cells occurred from day 100 onwards in patients under 60. However, the levels of sjTREC remained low for patients above 60. Further, chronic GVHD has a dramatic impact on thymic function, as observed after myeloablative conditioning.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal