Recent studies suggested that JAK2V617F mutation is frequent in patients with splanchnic vein thrombosis (SVT) but not in patients with other venous thromboembolic events (VTE). However, whether screening for the JAK2V617F mutation in VTE patients is justified remains unclear. Therefore, we performed a systematic review to assess the frequency of JAK2 mutation in VTE patients and the role of JAK2V617F mutation in the diagnosis of myeloproliferative neoplasms. MEDLINE and EMBASE databases were searched. Two reviewers independently performed study selection and extracted study characteristics. Pooled odds ratios of case-control studies and weighted mean proportion of the prevalence of JAK2V617F mutation of uncontrolled series were calculated. Twenty-four studies involving 3123 patients were included. Mean prevalence of JAK2 mutation was 32.7% (95% confidence interval, 25.5%-35.9%) in SVT patients. JAK2 mutation was associated with increased risk of SVT (odds ratio, 53.98; 95% confidence interval, 13.10-222.45). Mean prevalence of JAK2 mutation in other VTE patients was low (range, 0.88%-2.57%). Presence of JAK2V617F mutation in SVT patients was associated with a subsequent diagnosis of myeloproliferative neoplasm in many patients. JAK2 mutation is strongly associated with SVT, and routine screening of JAK2 mutation appears to be indicated in these patients.
Venous and arterial thrombosis are important causes of morbidity and mortality in patients with Philadelphia-negative (Ph−) myeloproliferative neoplasms (MPNs), polycythemia vera (PV), and essential thrombocythemia (ET).1 In particular, splanchnic vein thromboses (SVTs), which include portal vein thrombosis, mesenteric vein thrombosis, and thrombosis of the hepatic veins causing Budd-Chiari syndrome, are frequently the first manifestation of PV and ET.2 Overall, Ph− MPNs are among the commonest causes of Budd-Chiari syndrome and portal vein thrombosis, being found in up to 50% and 25% of the patients, respectively.3
The identification of occult MPNs in patients with venous thromboembolism (VTE) has traditionally been based on bone marrow biopsy findings and endogenous erythroid colony formation assessment.4 Both tests have significant limitations: bone marrow biopsy is invasive and its interpretation is, at best, semiquantitative; endogenous erythroid colony assessment is performed in only a few specialized centers, and its significance as a unique anomaly in patients with SVT has been disputed.5 These limitations have hindered diagnosis of underlying MPN and assessment of its influence on the outcome of VTE patients, particularly those with SVT.
The discovery of the gain-of-function JAK2V617F mutation, found in approximately 95% of patients with PV and in 50% of those with ET or primary myelofibrosis, has modified the diagnostic approach to Ph− MPNs.6,7 Several small series have suggested that JAK2V617F is found frequently in patients with SVT patients but not in VTE patients; many such patients have no other manifestations of an MPN.8 However, whether screening for the JAK2V617F mutation in patients presenting with venous thrombosis without overt MPD is justified remains unclear.
The aims of our systematic review were to assess the prevalence of the JAK2V617F mutation in patients' lower limb deep venous thrombosis and pulmonary embolism, and in patients with VTE in unusual sites (SVT, cerebral sinus, and vein thrombosis [CVT], upper limb deep venous thrombosis, and retinal vein occlusion [RVO]). Furthermore, we sought to examine the role of this mutation in the diagnosis of nonovert MPNs.
Methods
A protocol for this review was developed prospectively, detailing the specific objectives, criteria for study selection, approach to assess study quality, outcomes, and statistical methods.
Study identification
We attempted to identify all published studies that evaluated the prevalence of the JAK2 V617F mutation (homozygote and heterozygote) in patients with VTE in usual and unusual sites using the MEDLINE9 (1966 to October, week 2, 2008) and EMBASE10 (1980 to October, week 2, 2008) electronic databases. The search strategy was developed without any language restriction and used the subject headings presented in the “ Appendix.” We supplemented our search by manually reviewing abstract books from the Congress of the American Society of Hematology and the International Society on Thrombosis and Hemostasis (2005-2007), the reference lists of all retrieved articles, and contacting content experts for additional published or unpublished trials.
Study selection
Two reviewers (L.B., L.A.) performed study selection independently, with disagreements resolved through discussion and by the opinion of a third reviewer (F.D.), if necessary. Studies were included if they met the following criteria: (1) analysis of JAK2 mutation was performed according to established and commonly accepted criteria11 ; (2) patients were 18 years of age or older; and (3) at least 10 patients were included. To assess the agreement between reviewers for study selection, we used the κ statistic, which measures agreement beyond chance.12
Study validity assessment
The same 2 unmasked investigators independently completed the assessment of study validity. Because the use of quality scoring systems or quality scales in observational studies is controversial,13 the internal validity of each case-control study was evaluated considering 2 potential sources of bias.14 Studies were considered of low quality when subjects were arbitrarily excluded from either the case or control groups and when baseline characteristics of the control group (age, sex) were not matched with the characteristics of the patient group. Otherwise, studies were considered of higher quality.
Data extraction
L.A. and L.B. independently extracted data on study (year of publication, design, study center) and patient characteristics (number of subjects studied, mean age, variation in age, sex, and race). Furthermore, the prevalence of JAK2V617F mutation was assessed in all the studies in which a population of patients with VTE was considered. Disagreement was resolved by consensus and by opinion of a third reviewer (F.D.), if necessary. If the required data could not be located in the published report, we contacted the corresponding author, with a reminder sent after 15 days. The definition of overt or nonovert MPN and the definition of idiopathic or nonidiopathic SVT were based on the definitions used in each selected study.
Statistical analysis
Weighted mean proportion of the prevalence of JAK2 mutation was calculated using random-effects model. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated when studies compared the prevalence of JAK2 mutation in VTE patients and in controls. These data were pooled using a fixed-effects model (Mantel-Haenszel method)15 and comparing these findings with results obtained using a random-effects model (DerSimionan and Laird method).16 Statistical heterogeneity was evaluated using the I2 statistic, which assesses the appropriateness of pooling the individual study results.17 The I2 value provides an estimate of the amount of variance across studies resulting from heterogeneity rather than chance. P less than .05 was considered to denote statistically significant heterogeneity. When heterogeneity was present, we repeated the analyses removing one study at a time to assess the source of heterogeneity. The proportion of VTE in the different populations that could be attributed to JAK2 mutation (population-attributable risk) was estimated as follows:
Population-attributable risk = 100 × [prevalence(OR − 1)/prevalence(OR − 1) + 1]
For this calculation, we used the fixed-effects model, and we estimated the prevalence of exposure as the genotype frequency among control subjects. The presence of publication bias was explored using funnel plots of effect size against SE.18
Results
Study identification and selection
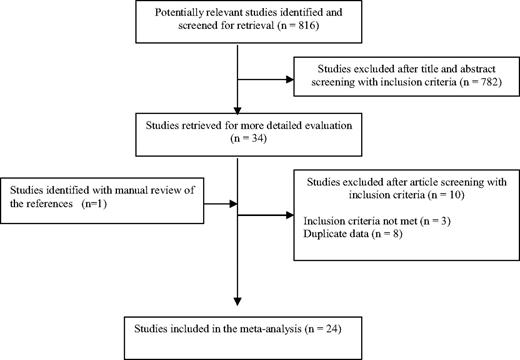
We identified 1036 potentially relevant studies from the following databases: 691 from EMBASE, 295 from MEDLINE, and 50 from abstracts books from the American Society of Hematology and International Society on Thrombosis and Hemostasis Congress. A total of 220 studies were duplicated, and 782 studies were excluded after title and abstract screening using predefined inclusion and exclusion criteria; the remaining 34 studies were retrieved in full for detailed evaluation.10,19,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,–51 One additional study was identified through manual review of references.52 The study identification and selection progression are summarized in Figure 1.
Of the 35 retrieved studies, 11 were excluded for the following reasons: 7 contained duplicated data19,22,26,28,29,32,39,,,,,,,,,,–50 and 320,33,38 included fewer than 10 patients. Twenty-four studies were therefore included in this systematic review.10,21,23,25,27,30,33,37,40,,,,,,,,–49,51,52 Interobserver agreement for study selection was excellent (κ = 0.96).
Study characteristics
Baseline characteristics of patients included in the studies are summarized in Table 1. All studies were written in English, and all studies analyzed the V617F mutation of JAK2; other mutations of JAK2 were not assessed. Studies ranged in size from 11 to 560 patients; a total of 3508 patients were included. Six case-control studies10,23,25,27,35,40 and 18 retrospective cohort studies21,24,30,31,34,36,37,41,,,,,,,–49,51,52 were included in our systematic review. Five studies enrolled patients consecutively.35,42,44,46,51 A few studies differentiated between patients with homozygote and heterozygote JAK2V617F mutation,24,34,35,41,43,44,49 and 2 studies provided data on patients with homozygote mutation JAK2V617F.24,,,,,,,,,,–35 Sixteen studies,10,21,23,–25,30,35,–37,40,43,44,46,47,49,53 including a total 831 patients, assessed the prevalence of JAK2V617F mutation in patients with SVT. Eight studies,21,27,34,37,40,–42,47 including 1293 patients, assessed the prevalence of JAK2V617F mutation in patients with deep vein thrombosis of the leg or pulmonary embolism. Six studies,21,24,40,41,45,51 for a total 241 patients, assessed the prevalence of JAK2V617F mutation in patients with CVT. Finally, 6 studies21,31,40,41,47,48 with a total 153 patients assessed the prevalence of JAK2V617F mutation in patients with RVO. No study assessed the JAK2V617F mutation in patients with upper limb deep venous thrombosis.
Baseline characteristics of patients included in the studies
| Study, date (reference no.) . | Study type . | Selected population . | Median age, y (range) . | No. of patients . | JAK2 mutation (homozygous or heterozygous) . | Population controls . |
|---|---|---|---|---|---|---|
| Rossi et al, 2007 (19) | Retrospective cohort | Patients with idiopathic VTE (absence of: known conditions of inherited or acquired thrombophilia; common acquired risk factors for VTE, malignancy, surgery, pregnancy, estrogen consumption, liver failure, and nephritic syndrome; overt Ph− CMPD). | 48 (5-84) | 139 (F/M 81/58) | 3 of 139 JAK2V617F (lower limb DVT 0 of 61, CVT 0 of 13, RVO 0 of 6, SVT 3 of 6, PE 0 of 53) | — |
| McMahon et al, 2007 (21) | Case-control | Patients with catastrophic intraabdominal venous thrombosis. | 47.5 (18-64) | 24¶ (F/M 10/14) | 5 of 24 JAK2V617F | 30 patients with hereditary pancreatitis (mutation in the PRSS1 gene); 0 of 30 JAK2V617F |
| De Stefano et al, 2007 (22) | Retrospective cohort | Patients with idiopathic SVT or CVT, excluding overt cancer. | — | 139 (94 SVT + 45 CVT) | 37 of 139 JAK2V617F (32 of 94 SVT and 5 of 45 CVT**) (27 of 37 were sequenced | — |
| Regina et al, 2007 (23) | Case-control | Patients with HVT or EHPVO in whom liver cirrhosis, infection, and neoplastic disease were excluded. | 39 (22-76) | 44 (F/M 21/23) | 8 of 44 JAK2V617F | |
| Patients with spontaneous DVT of the lower limbs. | 39 (22-76) | 44 (F/M 21/23) | 0 of 44 JAK2V617F | |||
| Remacha et al, 2007 (25) | Case-control | Patients with thrombosis in common locations (consecutive patients with a first thrombotic event < 70 years, excluding those with neoplastic disease, liver failure, nephrotic syndrome). | 48 ± 14 | 295 (F/M 162/133) | 1 of 295 JAK2V617F | 65 patients with other hematologic non-CMPD; 0 of 65 JAK2V617F |
| Boissinot et al, 2006 (28) | Retrospective cohort | Patients with SVT. | 46.8* | 45 (F/M 21/24) | 14 of 45 JAK2V617F | — |
| Patel et al, 2006 (8) | Case-control | Patients with idiopathic BCS, excluding secondary etiology: adult polycystic liver and renal disease, hepatic vein stenosis, inferior vena cava stenosis, Bechet disease, carcinoid tumor, malignant infiltration, hepatocellular carcinoma, pregnancy, sickle cell disease, ulcerative colitis, PV, hydatid liver disease. | 35.5 ± 13.3* | 41 (F/M 26/15) | 24 of 41 JAK2V617F; during follow-up, 11 of 41 developed CMPD; 10 of 11 JAK2V617F | 27 patients with nonthrombotic liver disease (autoimmune, acetaminophen overdose, Gilbert syndrome, and Wilson disease); 0 of 27 JAK2V617F |
| Héron et al, 2007 (29) | Retrospective cohort | Patients with a first or recurrent central or brunch RVO, excluding traumatic, inflammatory, or tumor-related local cause of RVO; history of cancer, CMPD, systemic immunoinflammatory disease, and overt organ failure. | 46.1 ± 11.5* (25-58)† | 11 | 0 of 11 JAK2V617F | — |
| Ugo et al, 2007 (32) | Retrospective cohort | Patients with first unprovoked VTE without major acquired risk factor: surgery, plaster cast, pregnancy or delivery in the past 3 months, cancer. | 73 (18-96) | 394 (F/M 226/168) | 6 of 394 JAK2V617F | — |
| Primignani et al, 2006 (33) | Case-control | Consecutive patients with EHPVO or BCS, excluding neoplastic disease and liver cirrhosis. None of the patients had prior history of CMPD. | 38 (13-72) | 93 (20 BCS + 73 EHPVO) (F/M 56/37) | 34 of 93 JAK2V617F (26 heterozygous, 8 homozygous) | 20 healthy subjects; 0 of 20 JAK2V617F |
| Kiladjian et al, 2008 (34) | Retrospective cohort | Patients with EHPVO or BCS, excluding neoplastic disease and liver cirrhosis. | BCS: 36 (27-46) PVT: 42 (30-57) | 241 (104 BCS + 137 EHPVO) (F/M 129/112) | 94 of 241 JAK2V617F (47 of 104; 47 of 137) | — |
| Abel et al, 2008 (35) | Retrospective cohort | Patients with documented venous thrombosis (DVT, PE, SVT), excluding neoplastic disease, CMPD, or HIT within 1 year of thrombosis. | 52 | 1 of 52 JAK2V617F (0 of 45 DVT of PE 1 of 7 SVT) | — | |
| Colaizzo et al, 2007 (38) | Case-control | Patients with SVT, RVO, CVT, or DVT, excluding cirrhosis or hepatocellular carcinoma. | SVT: 47 (10-86) RVO: 51 (20-81) CVT: 40 (13-55) DVT: 49 (12-81) | 139 SVT (F/M 83/56); 93 RVO (F/M 42/51); 45 CVT (F/M 31/14); 110 DVT (F/M 51/59) | 27 of 139 JAK2V617F (0 of 93 RVO, 0 of 45 CVT, 0 of 110 DVT) | 286 healthy subjects (F/M 163/119; median age, 44 years; range, 21-73 years); 0 of 286 JAK2V617F |
| Pardanani et al, 2008 (39) | Retrospective cohort | Patients with non-SVT and non-CMPD. | 56 (17-93)‡ | 303 (114 DVT, 95 PE, 50 DVT and PE, 10 RVO, 7 CVT, 27 other thromboses) | 4 of 303 JAK2V617F (1 of 10 RVO, 1 of 7 CVT and PE, 1 of 50 DVT and PE, 1 of 95 PE) | — |
| Sène et al, 2008 (40) | Retrospective color | Consecutive patients with venous thrombosis (lower limbs, inferior vena cava, arm, pulmonary arteries). | 45.8 ± 18 | 44 (F/M 23/21) | 0 of 44 JAK2V617F | — |
| Bayraktar et al, 2008 (41) | Retrospective color | Patients with chronic noncirrhotic PVT (chronic PVT: partial or total occlusion of the portal system known for > 6 months or as the presence of portal vein cavernous transformation). Patients with acute or subacute PVT (within 3 months), cirrhosis, or liver malignancy were excluded. | 44.9* (24-73) | 25 (F/M 16/9) | 6 of 25 JAK2V617F; all were heterozygous | — |
| Colaizzo et al, 2008 (42) | Retrospective cohort | Consecutive patients with BCS. | 35 (14-66) | 32 (F/M 23/9) | 11 of 32 JAK2V617F | — |
| Bellucci et al, 2008 (43) | Retrospective cohort | Patients with CVT without overt CMPD | 35.4 ± 12.9 | 87 (F/M 68/19) | 1 of 87 JAK2V617F | — |
| Garcés-Eisele et al, 2008 (44) | Retrospective cohort | Patients with at least 1 episode of venous thrombosis confirmed by phlebography or Doppler in the previous 30 days. Patients with overt malignancy, pregnancy, puerperium, oral contraceptives, or other conditions associated with secondary thrombophilia were excluded. | 77 (F/M 51/26) | 0 of 77 JAK2V617F (0 of 4 SV; 0 of 73 DVT) | ||
| Karimi et al, 2008 (45) | Retrospective cohort | Thrombotic IBD patients (22 CD and 26 UC). | 37.5§ | 36 | 0 of 36 JAK2 V617 F (0 of 30 DVT; 0 of 2; 0 of 2 RVO; 0 of 2 SVT) | — |
| Hermans et al, 2008 (46) | Retrospective cohort | Patients with idiopathic RVO. | 51* (20-80) | 31 (F/M 17/14) | 0 of 31 JAK2V617F | — |
| Goulding et al, 2008 (47) | Retrospective cohort | Patients with HVT (10) and PVT (10). Patients with thrombophila, pregnancy, malignancy, sepsis, OC, preexisting cirrhosis, and patients with overt CMPD at the time of diagnosis of thrombosis were excluded. | 41 (24-76) | 19 | 14 of 19 JAK2V617F; all were heterozygous | |
| Xavier et al, 2008 (49) | Retrospective cohort | Consecutive CVT patients without overt CMPD. | 28 (15-65) | 44 (F/M 30/14) | 0 of 44 JAK2V617F | |
| Smalberg et al, 2006 (50) | Retrospective cohort | Patients with BCS. | 26.3 | 17 (F/M 10/7) | 7 of 17 JAK2V617F | — |
| Study, date (reference no.) . | Study type . | Selected population . | Median age, y (range) . | No. of patients . | JAK2 mutation (homozygous or heterozygous) . | Population controls . |
|---|---|---|---|---|---|---|
| Rossi et al, 2007 (19) | Retrospective cohort | Patients with idiopathic VTE (absence of: known conditions of inherited or acquired thrombophilia; common acquired risk factors for VTE, malignancy, surgery, pregnancy, estrogen consumption, liver failure, and nephritic syndrome; overt Ph− CMPD). | 48 (5-84) | 139 (F/M 81/58) | 3 of 139 JAK2V617F (lower limb DVT 0 of 61, CVT 0 of 13, RVO 0 of 6, SVT 3 of 6, PE 0 of 53) | — |
| McMahon et al, 2007 (21) | Case-control | Patients with catastrophic intraabdominal venous thrombosis. | 47.5 (18-64) | 24¶ (F/M 10/14) | 5 of 24 JAK2V617F | 30 patients with hereditary pancreatitis (mutation in the PRSS1 gene); 0 of 30 JAK2V617F |
| De Stefano et al, 2007 (22) | Retrospective cohort | Patients with idiopathic SVT or CVT, excluding overt cancer. | — | 139 (94 SVT + 45 CVT) | 37 of 139 JAK2V617F (32 of 94 SVT and 5 of 45 CVT**) (27 of 37 were sequenced | — |
| Regina et al, 2007 (23) | Case-control | Patients with HVT or EHPVO in whom liver cirrhosis, infection, and neoplastic disease were excluded. | 39 (22-76) | 44 (F/M 21/23) | 8 of 44 JAK2V617F | |
| Patients with spontaneous DVT of the lower limbs. | 39 (22-76) | 44 (F/M 21/23) | 0 of 44 JAK2V617F | |||
| Remacha et al, 2007 (25) | Case-control | Patients with thrombosis in common locations (consecutive patients with a first thrombotic event < 70 years, excluding those with neoplastic disease, liver failure, nephrotic syndrome). | 48 ± 14 | 295 (F/M 162/133) | 1 of 295 JAK2V617F | 65 patients with other hematologic non-CMPD; 0 of 65 JAK2V617F |
| Boissinot et al, 2006 (28) | Retrospective cohort | Patients with SVT. | 46.8* | 45 (F/M 21/24) | 14 of 45 JAK2V617F | — |
| Patel et al, 2006 (8) | Case-control | Patients with idiopathic BCS, excluding secondary etiology: adult polycystic liver and renal disease, hepatic vein stenosis, inferior vena cava stenosis, Bechet disease, carcinoid tumor, malignant infiltration, hepatocellular carcinoma, pregnancy, sickle cell disease, ulcerative colitis, PV, hydatid liver disease. | 35.5 ± 13.3* | 41 (F/M 26/15) | 24 of 41 JAK2V617F; during follow-up, 11 of 41 developed CMPD; 10 of 11 JAK2V617F | 27 patients with nonthrombotic liver disease (autoimmune, acetaminophen overdose, Gilbert syndrome, and Wilson disease); 0 of 27 JAK2V617F |
| Héron et al, 2007 (29) | Retrospective cohort | Patients with a first or recurrent central or brunch RVO, excluding traumatic, inflammatory, or tumor-related local cause of RVO; history of cancer, CMPD, systemic immunoinflammatory disease, and overt organ failure. | 46.1 ± 11.5* (25-58)† | 11 | 0 of 11 JAK2V617F | — |
| Ugo et al, 2007 (32) | Retrospective cohort | Patients with first unprovoked VTE without major acquired risk factor: surgery, plaster cast, pregnancy or delivery in the past 3 months, cancer. | 73 (18-96) | 394 (F/M 226/168) | 6 of 394 JAK2V617F | — |
| Primignani et al, 2006 (33) | Case-control | Consecutive patients with EHPVO or BCS, excluding neoplastic disease and liver cirrhosis. None of the patients had prior history of CMPD. | 38 (13-72) | 93 (20 BCS + 73 EHPVO) (F/M 56/37) | 34 of 93 JAK2V617F (26 heterozygous, 8 homozygous) | 20 healthy subjects; 0 of 20 JAK2V617F |
| Kiladjian et al, 2008 (34) | Retrospective cohort | Patients with EHPVO or BCS, excluding neoplastic disease and liver cirrhosis. | BCS: 36 (27-46) PVT: 42 (30-57) | 241 (104 BCS + 137 EHPVO) (F/M 129/112) | 94 of 241 JAK2V617F (47 of 104; 47 of 137) | — |
| Abel et al, 2008 (35) | Retrospective cohort | Patients with documented venous thrombosis (DVT, PE, SVT), excluding neoplastic disease, CMPD, or HIT within 1 year of thrombosis. | 52 | 1 of 52 JAK2V617F (0 of 45 DVT of PE 1 of 7 SVT) | — | |
| Colaizzo et al, 2007 (38) | Case-control | Patients with SVT, RVO, CVT, or DVT, excluding cirrhosis or hepatocellular carcinoma. | SVT: 47 (10-86) RVO: 51 (20-81) CVT: 40 (13-55) DVT: 49 (12-81) | 139 SVT (F/M 83/56); 93 RVO (F/M 42/51); 45 CVT (F/M 31/14); 110 DVT (F/M 51/59) | 27 of 139 JAK2V617F (0 of 93 RVO, 0 of 45 CVT, 0 of 110 DVT) | 286 healthy subjects (F/M 163/119; median age, 44 years; range, 21-73 years); 0 of 286 JAK2V617F |
| Pardanani et al, 2008 (39) | Retrospective cohort | Patients with non-SVT and non-CMPD. | 56 (17-93)‡ | 303 (114 DVT, 95 PE, 50 DVT and PE, 10 RVO, 7 CVT, 27 other thromboses) | 4 of 303 JAK2V617F (1 of 10 RVO, 1 of 7 CVT and PE, 1 of 50 DVT and PE, 1 of 95 PE) | — |
| Sène et al, 2008 (40) | Retrospective color | Consecutive patients with venous thrombosis (lower limbs, inferior vena cava, arm, pulmonary arteries). | 45.8 ± 18 | 44 (F/M 23/21) | 0 of 44 JAK2V617F | — |
| Bayraktar et al, 2008 (41) | Retrospective color | Patients with chronic noncirrhotic PVT (chronic PVT: partial or total occlusion of the portal system known for > 6 months or as the presence of portal vein cavernous transformation). Patients with acute or subacute PVT (within 3 months), cirrhosis, or liver malignancy were excluded. | 44.9* (24-73) | 25 (F/M 16/9) | 6 of 25 JAK2V617F; all were heterozygous | — |
| Colaizzo et al, 2008 (42) | Retrospective cohort | Consecutive patients with BCS. | 35 (14-66) | 32 (F/M 23/9) | 11 of 32 JAK2V617F | — |
| Bellucci et al, 2008 (43) | Retrospective cohort | Patients with CVT without overt CMPD | 35.4 ± 12.9 | 87 (F/M 68/19) | 1 of 87 JAK2V617F | — |
| Garcés-Eisele et al, 2008 (44) | Retrospective cohort | Patients with at least 1 episode of venous thrombosis confirmed by phlebography or Doppler in the previous 30 days. Patients with overt malignancy, pregnancy, puerperium, oral contraceptives, or other conditions associated with secondary thrombophilia were excluded. | 77 (F/M 51/26) | 0 of 77 JAK2V617F (0 of 4 SV; 0 of 73 DVT) | ||
| Karimi et al, 2008 (45) | Retrospective cohort | Thrombotic IBD patients (22 CD and 26 UC). | 37.5§ | 36 | 0 of 36 JAK2 V617 F (0 of 30 DVT; 0 of 2; 0 of 2 RVO; 0 of 2 SVT) | — |
| Hermans et al, 2008 (46) | Retrospective cohort | Patients with idiopathic RVO. | 51* (20-80) | 31 (F/M 17/14) | 0 of 31 JAK2V617F | — |
| Goulding et al, 2008 (47) | Retrospective cohort | Patients with HVT (10) and PVT (10). Patients with thrombophila, pregnancy, malignancy, sepsis, OC, preexisting cirrhosis, and patients with overt CMPD at the time of diagnosis of thrombosis were excluded. | 41 (24-76) | 19 | 14 of 19 JAK2V617F; all were heterozygous | |
| Xavier et al, 2008 (49) | Retrospective cohort | Consecutive CVT patients without overt CMPD. | 28 (15-65) | 44 (F/M 30/14) | 0 of 44 JAK2V617F | |
| Smalberg et al, 2006 (50) | Retrospective cohort | Patients with BCS. | 26.3 | 17 (F/M 10/7) | 7 of 17 JAK2V617F | — |
SVT indicates splanchnic vein thrombosis; BCS, Budd-Chiari syndrome; EHPVO, extrahepatic portal vein obstruction; CMPD, chronic myeloproliferative disease; PV, polycythemia vera; CVT, cerebral venous thrombosis; HVT, hepatic venous thrombosis; DVT, deep vein thrombosis; MVT, mesenteric vein thrombosis; VTE, venous thromboembolism; PMVT, portal and mesenteric venous thrombosis; RVO, retinal vein occlusion; HIT, heparin-induced thrombocytopenia; US, ultrasonography; CT, computed tomography; MR, magnetic resonance; PE, pulmonary embolism; MF, idiopathic myelofibrosis; CML, chronic myeloid leukemia; PVT, portal vein thrombosis; ET, essential thrombocythemia; IBD, inflammatory bowel disease; CD, Crohn disease; UC, ulcerative colitis; F, female; M, male; and —, not applicable.
Mean or mean ± SD.
Age referred to 12 patients.
Referred to 439 patients.
Median age of onset of IBD.
¶Two patients had also arterial superior mesenteric thrombosis.
Data on patients with CVT were supplemented with data of a more recent publication; 6 of 52 patients with CVT were positive for JAK2 V617F mutation (xx).
Study quality
Patients with SVT
A total of 280 of 831 patients with SVT had the JAK2V617F mutation, for a mean prevalence of 32.7% (95% CI, 25.5%-35.9%). Five studies provided the prevalence of the JAK2V617F mutation in patients with idiopathic SVT10,21,36,37,49 ; the mutation was present in 49.0% (95% CI, 32.9%-65.1%) of such patients. Ten studies21,23,–25,35,37,40,43,44,52 provided separate data on the rate of diagnosis of myeloproliferative disorder in patients with JAK2 mutation at the time of diagnosis of SVT (77 of 131 patients; mean prevalence, 59.5%; 95% CI, 51.3%-67.5%), and 5 studies provided data on the rate of diagnosis of myeloproliferative disorder during the follow-up period in patients with JAK2 mutation without a diagnosis of myeloproliferative disorder at the time of SVT diagnosis (21 of 41 patients; mean rate, 52.4%; 95% CI, 38.0%-66.5%).21,23,25,40,49
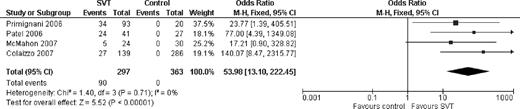
Four case-control studies evaluated the association between JAK2V617F mutation and SVT.10,23,35,40 Cases were composed by patients with SVT, whereas controls were composed by healthy subjects and by subjects with nonthrombotic liver and pancreatic disease. These studies included 297 cases and 363 controls. The JAK2V617F mutation was found significantly more often in patients with SVT than those without (OR, 53.98; 95% CI, 13.10-222.45; Figure 2), suggesting a strong association between the mutation and SVT. There was no heterogeneity among the studies (I2 = 0%). The analysis was repeated using the random-effects model, which yielded similar results (OR, 46.88; 95% CI, 11.21-196.15). The estimated attributable risk of SVT conferred by JAK2V617F mutation was 12.74% in this pooled cohort.
Odds ratio for the association between splanchnic vein thrombosis and JAK2 V617F mutation.
Odds ratio for the association between splanchnic vein thrombosis and JAK2 V617F mutation.
Patients with VTE in other sites
Ten of 1293 patients with deep vein thrombosis of the lower limbs or pulmonary embolism were found to have JAK2V617F mutation for a mean prevalence of 0.88% (95% CI, 0.44%-1.45%).21,27,34,37,40,42,47 Eight of 248 patients with CVT had JAK2V617F mutation, for a mean prevalence of 2.57% (95% CI, 0.97%-4.91%).21,24,40,41,45,51 One of 153 patients with RVO had JAK2V617F mutation, for a mean prevalence of 0.99% (95% CI, 0.05%-3.20%).21,31,40,41,47,48
Discussion
This is the first systematic review and meta-analysis that assessed the role of JAK2 mutation in patients with venous thrombosis. The results of this study indicate that the prevalence of this mutation is high in patients with SVT. On the other hand, we found the mutation to be no more common in patients with venous thrombosis at other sites than it is in patients with neither venous thrombosis nor known MPN.53 The meta-analysis of case-control studies found a strong association between JAK2V617F mutation and SVT, with an OR greater than 50.0, suggesting that a high proportion of SVTs can be associated with the presence of JAK2 mutation. Finally, the concomitant presence of JAK2 mutation in patients with SVT was associated with a subsequent diagnosis of an occult myeloproliferative disease in a large proportion of patients both at the time of SVT diagnosis and after long-term follow-up, suggesting both the role of the presence of JAK2 mutation as a marker of latent myeloproliferative disorders and that SVT commonly occurs as the first manifestation of MPN.
Taken together, these results suggest that, in general, patients with VTE should not be screened for the presence of JAK2 mutation. This screening appears to be justified in the population of patients with SVT, in whom the presence of JAK2 mutation is higher than 30% and in whom the finding of this mutation is a strong predictor of a subsequent diagnosis of an MPN. This is particularly relevant given that, in these patients, the concomitant presence of portal hypertension and hypersplenism could mask the increase in blood cell counts, even in the presence of ongoing myeloproliferation, thus making clinical suspicion more difficult.54 Whether the screening for JAK2 mutation could be justified also in patients with CVT remains controversial. Our results suggest a slight increase in the prevalence of the mutation in this patient population; however, the number of evaluated patients is small and the CI is thus too wide to allow any meaningful conclusion. Larger studies would be required to confirm or refute such an association.
Searching for an occult MPN in patients presenting with SVT, in particular, when other, major triggering factors are absent appears appropriate given that several studies have found MPN as one of the most common causes of SVT.55 However, routine screening with invasive and expensive procedures, such as bone marrow biopsy and endogenous erythroid colony formation assessment, may not be cost-effective if proposed to all such patients, in particular, in the absence of other specific signs of MPN, such as changes in blood cell counts. Routine testing for JAK2 mutation should identify those patients for whom additional investigation is warranted and may also prevent the need for additional investigation in some circumstances. Furthermore, according to the revised World Health Organization diagnostic criteria, invasive tests are not strictly necessary to diagnose PV in the presence of JAK2 mutation, and the presence of high hematocrit values in concomitance with serum erythropoietin level below the reference range for normal may be sufficient.56
Why the JAK2 mutation is so strongly associated with SVT is unknown. The mutation causes the constitutive activation of JAK2, which in turn results in cytokine-independent myeloproliferation, mobilization of blood cell progenitors, and the spontaneous formation of endogenous erythroid colonies leading to the development of a myeloproliferative disorder.57 Whether all these abnormalities also induce a hypercoagulable state will need to be determined by future studies. The reason for the specific association between JAK2 mutation and this unusual site of thrombosis could also be explained by the effects of the disease in the splanchnic system, possibly affecting the flow of the splanchnic venous bed. However, the exact mechanisms underlying these changes remain to be established.
Our systematic review has several potential limitations. First, our meta-analysis was restricted to case-control studies, and the application of formal meta-analytic methods to observational studies is controversial because bias implicit in the study design may misrepresent the strength of associations within the data.17 Second, studies included in our meta-analysis have different inclusion and exclusion criteria, and to combine results across studies may be inappropriate. However, the heterogeneity between the studies, calculated using the I2 statistic, was extremely low. Furthermore, when we repeated the analysis using a random-effects model, an approach that accounts for some of the variance between studies, we found similar results. Third, the importance of other inherited or acquired risk factors for thrombosis (in addition to the JAK2 mutation) could not be assessed as relevant data were not reported in the contributing articles. Thus, whether the presence of other risk factors contributes to the risk of SVT in patients with the JAK2 mutation remains unknown. Fourth, there are too few studies to assess the role of other less frequent mutations of JAK2 and to distinguish the risk of venous thrombosis in patients with heterozygous and homozygous V617F mutation of JAK2. Furthermore, given the low quality of case-control studies included in our systematic review, our findings should be interpreted with caution. Last, because there were too few case-control studies, the presence of publication bias could not be evaluated. However, given the magnitude of the association and the homogeneity of results in different studies, it is extremely doubtful that unpublished studies that did not find an association between SVT and JAK2 mutation, if really exist, could substantially modify our results.
In conclusion, the JAK2 mutation is strongly associated with SVT. Because the presence of JAK2 mutation is also a strong predictor of a subsequent diagnosis of occult MPNs and MPNs are among the most common causes of SVT, routine screening of JAK2 mutation appears to be indicated in patients presenting with SVT. This suggestion does not apply to patients presenting with VTE in other sites because the observed prevalence of this mutation was similar to the prevalence reported in the general population. Future studies are necessary to evaluate why SVT occurs in patients with MPN, the association of SVT, and other less frequent mutations of JAK2, and to better define the risk of venous thrombosis in patients with heterozygous and homozygous V617F mutation of JAK2.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: F.D. handled conception and design, analyzed and interpreted the data, drafted the article, critically revised the article for important intellectual content, gave final approval of the article, provided administrative, technical, or logistic support, and collected and assembled the data; A.S. and W.A. handled conception and design, analyzed and interpreted the data, drafted the article, critically revised the article for important intellectual content, and gave final approval of the article; L.B. and L.A. drafted the article, gave final approval of the article, and collected and assembled the data; and L.C., M.C., and A.M.G. drafted the article, critically revised the article for important intellectual content, and gave final approval of the article.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Francesco Dentali, Department of Clinical Medicine, University of Insubria, Viale Borri 57, Varese, 21100, Italy; e-mail: fdentali@libero.it.
Appendix: Medline search strategy
Database: Ovid MEDLINE(R), 1950 to October (Week 2) 2008
Janus Kinase 2/ (2301)
Portal Vein/ (15 338)
Budd-Chiari Syndrome/ (2472)
Mesenteric Veins/ (3651)
Mesenteric Vascular Occlusion/ (3661)
Venous Thrombosis/ (12 123)
Venous Thromboembolism/ (433)
Thromboembolism/ (17 903)
Thrombosis/ (46 277)
Pulmonary Embolism/ (26 470)
Pulmonary Embolism/ (26 470)
Intracranial Thrombosis/ (1059)
Cardiovascular Diseases/ (65 129)
2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 (179271)
1 and 14 (74)
Polycythemia Vera/ (4496)
Thrombocythemia, Hemorrhagic/ (1711)
16 or 17 (5833)
1 and 18 (264)
15 or 19 (295)