Monoclonal gammopathy of undetermined significance (MGUS) is a premalignant plasma-cell proliferative disorder associated with a life-long risk of progression to multiple myeloma (MM). It is not known whether MM is always preceded by a premalignant asymptomatic MGUS stage. Among 77 469 healthy adults enrolled in the nationwide population-based prospective Prostate, Lung, Colorectal, and Ovarian (PLCO) Cancer Screening Trial, we identified 71 subjects who developed MM during the course of the study in whom serially collected (up to 6) prediagnostic serum samples obtained 2 to 9.8 years prior to MM diagnosis were available. Using assays for monoclonal (M)–proteins (electrophoresis/immunofixation) and kappa-lambda free light chains (FLCs), we determined longitudinally the prevalence of MGUS and characterized patterns of monoclonal immunoglobulin abnormalities prior to MM diagnosis. MGUS was present in 100.0% (87.2%-100.0%), 98.3% (90.8%-100.0%), 97.9% (88.9%-100.0%), 94.6% (81.8%-99.3%), 100.0% (86.3%-100.0%), 93.3% (68.1%-99.8%), and 82.4% (56.6%-96.2%) at 2, 3, 4, 5, 6, 7, and 8+ years prior to MM diagnosis, respectively. In approximately half the study population, the M-protein concentration and involved FLC-ratio levels showed a yearly increase prior to MM diagnosis. In the present study, an asymptomatic MGUS stage consistently preceded MM. Novel molecular markers are needed to better predict progression to MM in patients with MGUS.
Introduction
Multiple myeloma (MM) is a clonal plasma-cell proliferative disorder with a median survival of approximately 4 years.1 Almost 19 900 new MM cases and 10 700 MM deaths are expected in the United States during 2008.2 Monoclonal gammopathy of undetermined significance (MGUS) is one of the most common premalignant disorders in Western countries, with a prevalence of 3.2% in the white general population 50 years of age or older.3 It is an asymptomatic condition characterized by the presence of a monoclonal immunoglobulin (M-protein) in the absence of any clinical signs or symptoms of MM or other lymphoproliferative malignancies.4,5
Long-term follow-up studies of MGUS patients show an excess risk of developing MM.6 However, a key gap in our understanding is whether MM is always preceded by MGUS, or if MM typically arises de novo. This knowledge is critically important in understanding the pathogenesis of MM and to develop preventive strategies. We hypothesize that a premalignant plasma-cell proliferative stage characterized by asymptomatic M-protein production, clinically defined as MGUS, is present in all patients with MM years prior to the development of the malignancy. The confirmation of this hypothesis would emphasize the need to focus on identifying risk factors for MGUS and to improve our knowledge on underlying mechanisms of transformation from MGUS to MM, with the aim to define better predictive markers of progression and to develop chemopreventive approaches.
Thus far, it has been impossible to determine whether a protracted premalignant phase MGUS precedes MM in all patients. Taking advantage of the large nationwide US PLCO (Prostate, Lung, Colorectal, and Ovarian) Cancer Screening Trial,7 we used a unique study design to conduct the first prospective study to address this question. Among 77 469 persons in the screened arm who were cancer-free at baseline, we identified 71 subjects who developed MM during the course of the study in whom serially collected prediagnostic serum samples obtained at least 2 years (up to 9.8 years) prior to MM diagnosis were available. Using multiple prediagnostic blood samples (up to 6 samples) obtained annually in the same subject, we applied serum protein electrophoresis, immunofixation, and kappa-lambda free light chain (FLC) assays to define the prevalence of MGUS prior to the diagnosis of MM, and characterized longitudinally patterns of M-protein abnormalities prior to MM diagnosis.
Methods
Study population, MM patients, and sample handling
The PLCO Cancer Screening Trial study population has been described previously.7 Briefly, more than 150 000 people aged 55 to 74 years were randomized from 1992 to 2001 to undergo a specific cancer screening regimen (screening arm) or receive routine medical care to evaluate the effects of screening on disease-specific mortality. Participants randomized to the screening arm underwent screening exams for the detection of prostate, lung, colorectal, and ovarian cancer. In addition, they provided annual blood samples (for 6 years) for research purposes. At baseline, study participants provided written, informed consent in accordance with the Declaration of Helsinki and completed a demographic and risk factor questionnaire.8 Information on incident cancers (type and date) was obtained prospectively using standardized questionnaires that were mailed out to all study participants on an annual basis. For all reported cancers, trained PLCO data abstracters reviewed and confirmed each case.
The study population for this investigation was drawn from the 77 469 participants in the screening arm. We identified a total of 106 incident MM cases in the database; 101 had given their consent to participate in research studies. Of these, 86 persons had available prediagnostic serum samples. To eliminate the influence of undiagnosed MM, we defined study subjects as eligible only if they had serum samples obtained at least 2 years prior to date of MM diagnosis (n = 71).
Given the average survival of MM during the years of the PLCO study was 3 to 4 years, we considered the detection of M-proteins 2 or more years prior to the diagnosis of MM as being indicative of a premalignant stage, rather than early undiagnosed MM, which without therapy would have almost certainly manifested clinically over that length of time. We recognized that a small percentage of patients we considered as MGUS may meet criteria for the more advanced premalignant stage termed smoldering MM, but for the purposes of this study our interest was to determine whether a premalignant asymptomatic stage preceded all cases of MM, regardless of whether that stage met the clinical diagnosis of MGUS or smoldering MM.
For all cases, serum samples (0.5 mL) stored in liquid nitrogen freezers were thawed and used for electrophoresis, immunofixation, and FLC assays (described in “Laboratory tests”).
This study was conducted according to a protocol approved by the Institutional Review Boards of the National Cancer Institute and the 10 screening centers.
Laboratory tests
For all cases, serum samples (0.5 mL) stored in liquid nitrogen freezers were thawed and processed and analyzed in an identical fashion in the Mayo Clinic Protein Immunology Laboratory (Rochester, MN).9 Electrophoresis was performed on agarose gel (REP; Helena Laboratories, Beaumont, TX). The agarose strip was inspected by a technician and by 2 of the authors (R.A.K. and J.A.K.). In parallel, we assessed all serum samples using immunofixation (Hydrasys and Hydragel; Sebia, Norcross, GA). Levels of FLCs were determined in all study samples using the FLC assay (Freelite; The Binding Site, Birmingham, United Kingdom) performed on a Dade-Behring Nephelometer (Deerfield, IL).10,–12 It consists of 2 separate measurements, one to detect free-kappa (normal range, 3.3-19.4 mg/L) and the other to detect free-lambda (normal range, 5.7-26.3 mg/L) light chains.9 In addition to measuring the absolute levels of FLC, the test also allowed us to assess presence/absence of clonality based on the ratio of kappa-lambda light chain levels (normal range, 0.26-1.65).
Statistical methods
Crude MGUS prevalence was estimated dividing the number of persons affected by MGUS by the total number of persons at risk. Exact 95% binomial confidence intervals (CIs) were computed for estimates of proportions. M-protein and FLC levels were transformed to be normally distributed. We analyzed the observed data and then also imputed MGUS status for those who had missing values by simply using the last observed value prior to diagnosis. We did not impute any missing values at the time points beyond the closest time to diagnosis. Linear regression models were used to test for trend in M-protein concentrations and FLC levels over time. We used generalized estimation equations (GEEs) to take into account the correlations between observations on the same subject.13 We used the independence working correlation matrices in the calculations; other working correlations yielded similar results, however. Further, using descriptive statistics, we evaluated variations in M-protein and FLC levels in individual patients.
Results
A total of 71 MM patients (median age, 70 years; 71.4% males) with available stored prediagnostic serum obtained 2 or more years prior to MM diagnosis were included in the study (Table 1). On average, study subjects had available 3 (range, 1-6) prediagnostic serum samples. The median time between the first and the last prediagnostic blood draw in relation to a subsequent MM diagnosis was 59 (range, 29-118) months and 32 (range, 24-84) months, respectively.
Patients' characteristics
| Variable . | No. . |
|---|---|
| Total, no. (%) | 71 (100) |
| Median age at MM diagnosis, y (range) | 70 (58-81) |
| Male sex, no. (%) | 50 (71.4) |
| Race/ethnicity, no. (%) | |
| White | 65 (92.9) |
| African American | 3 (4.3) |
| Pacific Islanders | 1 (1.4) |
| Hispanic | 1 (1.4) |
| Calendar year at MM diagnosis, median (range) | 2002 (1997-2005) |
| Latency between blood draw and subsequent MM dx (mo), median (range)* | |
| First prediagnostic blood draw | 59 (29-118) |
| Last prediagnostic blood draw | 32 (24-84) |
| Median number (range) of available prediagnostic serum samples per persons† | 3 (1-6) |
| Variable . | No. . |
|---|---|
| Total, no. (%) | 71 (100) |
| Median age at MM diagnosis, y (range) | 70 (58-81) |
| Male sex, no. (%) | 50 (71.4) |
| Race/ethnicity, no. (%) | |
| White | 65 (92.9) |
| African American | 3 (4.3) |
| Pacific Islanders | 1 (1.4) |
| Hispanic | 1 (1.4) |
| Calendar year at MM diagnosis, median (range) | 2002 (1997-2005) |
| Latency between blood draw and subsequent MM dx (mo), median (range)* | |
| First prediagnostic blood draw | 59 (29-118) |
| Last prediagnostic blood draw | 32 (24-84) |
| Median number (range) of available prediagnostic serum samples per persons† | 3 (1-6) |
dx indicates diagnosis.
Latency interval (mo) between the first and the last prediagnostic blood draw in relation to a subsequent MM diagnosis.
Blood samples were prospectively collected on an annual basis; blood was drawn up to 6 sequential years for each individual.
Prevalence of MGUS prior to multiple myeloma diagnosis
In our study, MGUS was defined as having an M-protein (detectable by electrophoresis or immunofixation), an abnormal FLC-ratio, or both. We used 2 approaches to define the prevalence of MGUS prior to MM diagnosis. In the first analysis (“main analysis”), the number of subjects at risk was based on the actual available serum samples at a given time point at least 2 years prior to MM diagnosis. In the secondary analysis (“imputed analysis”), we assumed a subsequent test to be positive if it was missing and if an earlier test was positive.
As shown in Table 2, in the main analysis, the prevalence of MGUS was 100.0% (95% CI: 87.2%-100.0%), 98.3% (90.8%-100.0%), 97.9% (88.9%-100.0%), 94.6% (81.8%-99.3%), 100.0% (86.3%-100.0%), 93.3% (68.1%-99.8%), and 82.4% (56.6%-96.2%) at 2, 3, 4, 5, 6, 7, and 8+ years prior to MM diagnosis, respectively (ptrend = .32). For the imputed data, the corresponding prevalence rates for MGUS were similar (Table 2).
Prevalence (%) and 95% binomial confidence intervals (CIs) of serum protein abnormalities year by year prior to multiple myeloma diagnosis
| Blood draw prior to multiple myeloma diagnosis, y . | M-spike* . | Abnormal kappa-lambda FLC-ratio† . | MGUS‡ . | |||
|---|---|---|---|---|---|---|
| n/N . | % (95% CI) . | n/N . | % (95% CI) . | n/N . | % (95% CI) . | |
| By year§ | ||||||
| 2 | 25/27 | 92.6 (75.7-99.1) | 23/27 | 85.2 (66.3-95.8) | 27/27 | 100.0 (87.2-100.0) |
| 3 | 54/58 | 93.1 (83.3-98.1) | 46/58 | 79.3 (66.7-88.8) | 57/58 | 98.3 (90.8-100.0) |
| 4 | 45/48 | 93.8 (82.8-98.7) | 29/46 | 63.0 (47.6-76.8) | 47/48 | 97.9 (88.9-100.0) |
| 5 | 34/37 | 91.9 (78.1-98.3) | 25/37 | 67.6 (50.2-82.0) | 35/37 | 94.6 (81.8-99.3) |
| 6 | 25/25 | 100.0 (86.3-100.0) | 19/25 | 76.0 (54.9-90.6) | 25/25 | 100.0 (86.3-100.0) |
| 7 | 14/15 | 93.3 (68.1-99.8) | 11/15 | 73.3 (44.9-92.2) | 14/15 | 93.3 (68.1-99.8) |
| 8 or more | 13/17 | 76.5 (50.1-93.2) | 8/17 | 47.1 (23.0-72.2) | 14/17 | 82.4 (56.6-96.2) |
| Trend test | P = .60 | P = .12 | P = .32 | |||
| By year‖ | ||||||
| 2 | 64/70 | 91.4 (82.6-96.8) | 52/70 | 74.3 (62.4-84.0) | 68/70 | 97.1 (90.1-99.7) |
| 3 | 61/67 | 91.0 (81.5-96.6) | 50/67 | 74.6 (62.5-84.5) | 65/67 | 97.0 (89.6-99.6) |
| 4 | 48/53 | 90.6 (79.3-96.9) | 31/52 | 59.6 (45.1-73.0) | 51/53 | 96.2 (87.0-99.5) |
| 5 | 36/41 | 87.8 (73.8-95.9) | 25/41 | 61.0 (44.5-84.1) | 38/41 | 92.7 (80.1-98.5) |
| 6 | 26/28 | 92.9 (76.5-99.1) | 19/28 | 67.9 (47.7-84.1) | 27/28 | 96.4 (81.7-99.9) |
| 7 | 14/16 | 87.5 (61.7-98.5) | 11/16 | 68.8 (41.3-89.0) | 15/16 | 93.8 (69.8-99.8) |
| 8 or more | 13/17 | 76.5 (50.1-93.2) | 8/17 | 47.1 (23.0-72.2) | 14/17 | 82.4 (56.6-96.2) |
| Trend test | P = .43 | P = .13 | P = .34 | |||
| Blood draw prior to multiple myeloma diagnosis, y . | M-spike* . | Abnormal kappa-lambda FLC-ratio† . | MGUS‡ . | |||
|---|---|---|---|---|---|---|
| n/N . | % (95% CI) . | n/N . | % (95% CI) . | n/N . | % (95% CI) . | |
| By year§ | ||||||
| 2 | 25/27 | 92.6 (75.7-99.1) | 23/27 | 85.2 (66.3-95.8) | 27/27 | 100.0 (87.2-100.0) |
| 3 | 54/58 | 93.1 (83.3-98.1) | 46/58 | 79.3 (66.7-88.8) | 57/58 | 98.3 (90.8-100.0) |
| 4 | 45/48 | 93.8 (82.8-98.7) | 29/46 | 63.0 (47.6-76.8) | 47/48 | 97.9 (88.9-100.0) |
| 5 | 34/37 | 91.9 (78.1-98.3) | 25/37 | 67.6 (50.2-82.0) | 35/37 | 94.6 (81.8-99.3) |
| 6 | 25/25 | 100.0 (86.3-100.0) | 19/25 | 76.0 (54.9-90.6) | 25/25 | 100.0 (86.3-100.0) |
| 7 | 14/15 | 93.3 (68.1-99.8) | 11/15 | 73.3 (44.9-92.2) | 14/15 | 93.3 (68.1-99.8) |
| 8 or more | 13/17 | 76.5 (50.1-93.2) | 8/17 | 47.1 (23.0-72.2) | 14/17 | 82.4 (56.6-96.2) |
| Trend test | P = .60 | P = .12 | P = .32 | |||
| By year‖ | ||||||
| 2 | 64/70 | 91.4 (82.6-96.8) | 52/70 | 74.3 (62.4-84.0) | 68/70 | 97.1 (90.1-99.7) |
| 3 | 61/67 | 91.0 (81.5-96.6) | 50/67 | 74.6 (62.5-84.5) | 65/67 | 97.0 (89.6-99.6) |
| 4 | 48/53 | 90.6 (79.3-96.9) | 31/52 | 59.6 (45.1-73.0) | 51/53 | 96.2 (87.0-99.5) |
| 5 | 36/41 | 87.8 (73.8-95.9) | 25/41 | 61.0 (44.5-84.1) | 38/41 | 92.7 (80.1-98.5) |
| 6 | 26/28 | 92.9 (76.5-99.1) | 19/28 | 67.9 (47.7-84.1) | 27/28 | 96.4 (81.7-99.9) |
| 7 | 14/16 | 87.5 (61.7-98.5) | 11/16 | 68.8 (41.3-89.0) | 15/16 | 93.8 (69.8-99.8) |
| 8 or more | 13/17 | 76.5 (50.1-93.2) | 8/17 | 47.1 (23.0-72.2) | 14/17 | 82.4 (56.6-96.2) |
| Trend test | P = .43 | P = .13 | P = .34 | |||
Detectable by electrophoresis, immunofixation, or both.
Normal reference range: 0.26-1.65.
Defined as having evidence of an M-spike (detectable by electrophoresis, immunofixation, or both), an abnormal FLC-ratio (<0.26 or >1.65), or both.
Individuals at risk were based on an actual available serum sample at a given time point (eg, 2 years prior to MM diagnosis) and the results were based on the outcome of assays from that same sample.
Individuals at risk were based on imputed statistical modeling (see further details in “Statistical methods”), where individuals with an available serum samples and with an abnormal finding in an earlier year (eg, 5 years prior to multiple myeloma diagnosis there was evidence of an M-spike) were set to be at risk and to have evidence of an M-spike in the following years (ie, 4, 3, and 2 years prior to MM diagnosis). These models were based on the assumption that once these protein abnormalities are present they do not entirely disappear.
We also defined the prevalence of having an M-protein (detected by electrophoresis, immunofixation, or both) and an abnormal kappa-lambda FLC-ratio separately (Table 2) among subjects subsequently diagnosed with MM. In the main analysis, the prevalence of M-proteins was 92.6% (75.7%-99.1%), 93.1% (98.1%-98.1%), 93.8% (82.8%-98.7%), 91.9% (78.1%-98.3%), 100.0% (86.3%-100.0%), 93.3% (68.1%-99.8%), and 76.5% (50.1%-93.2%) at 2, 3, 4, 5, 6, 7, and 8+ years prior to MM diagnosis, respectively (ptrend = .60). The prevalence of an abnormal kappa-lambda FLC-ratio for the corresponding years was 85.2% (66.3%-95.8%), 79.3% (66.7%-88.8%), 63.0% (47.6%-76.8%), 67.6% (50.2%-82.0%), 76.0% (54.9%-90.6%), 73.3% (44.9%-92.2%), and 47.1% (23.0%-72.2%), respectively (ptrend = .12). Again, analyses based on imputed data yielded similar results (Table 2).
Characteristics and variations of serum protein abnormalities over time prior to multiple myeloma diagnosis
To demonstrate M-protein and FLC patterns prior to MM diagnosis, we defined characteristics of serum protein abnormalities at given time points (2, 3, 4, 5, 6, 7, and 8+ years prior to MM diagnosis) on a group level. In parallel, to explore the possibility that there might be patients with stable protein levels prior to MM while others have evidence of progressive protein abnormalities, we evaluated longitudinal protein variations in individual study subjects.
The median for M-protein concentration exhibited a year-by-year (ptrend = .025) increase; at 8+ and 2 years prior to MM diagnosis, the median (range) concentration was 0.9 (0.5-1.8) and 1.6 (0.4-3.7) grams per deciliter (g/dL), respectively (Table 3). However, when we assessed FLC levels over time, a statistical association was absent (Table 3).
Median (range) M-protein concentration and measures of free light chains year by year prior to multiple myeloma diagnosis
| Blood draw prior to multiple myeloma diagnosis, y . | M-protein concentration* (g/dL) . | Involved FLC-ratio† . | Involved-uninvolved FLC concentration,† mg/dL . | Involved FLC concentration,† mg/dL . | ||
|---|---|---|---|---|---|---|
| n . | Median (range) . | n . | Median (range) . | Median (range) . | Median (range) . | |
| By year | ||||||
| 2 | 24 | 1.6 (0.4-3.7) | 23 | 12.1 (2.3-138.4) | 7.8 (0.6-61.9) | 8.5 (0.9-62.3) |
| 3 | 47 | 1.3 (0.5-3.1) | 46 | 10.7 (1.7-285.7) | 7.3 (0.6-118.2) | 8.3 (1.0-119.0) |
| 4 | 37 | 1.1 (0.5-3.9) | 30 | 11.3 (1.8-1428.0) | 5.1 (0.6-326.8) | 6.1 (0.9-327.0) |
| 5 | 26 | 1.2 (0.6-3.8) | 25 | 12.5 (1.7-4042.6) | 9.0 (0.6-322.9) | 9.2 (1.5-323.0) |
| 6 | 20 | 1.2 (0.6-3.6) | 19 | 14.3 (1.7-907.5) | 10.7 (0.6-205.8) | 11.1 (1.5-206.0) |
| 7 | 11 | 1.3 (0.7-3.5) | 11 | 32.6 (1.8-677.9) | 12.9 (0.9-180.7) | 14.0 (2.0-181.0) |
| 8 or more | 10 | 0.9 (0.5-1.8) | 8 | 19.4 (2.6-107.1) | 12.0 (1.8-32.7) | 13.0 (3.0-33.0) |
| Trend test | P = .025 | P = .35 | –‡ | P = .30 | ||
| Blood draw prior to multiple myeloma diagnosis, y . | M-protein concentration* (g/dL) . | Involved FLC-ratio† . | Involved-uninvolved FLC concentration,† mg/dL . | Involved FLC concentration,† mg/dL . | ||
|---|---|---|---|---|---|---|
| n . | Median (range) . | n . | Median (range) . | Median (range) . | Median (range) . | |
| By year | ||||||
| 2 | 24 | 1.6 (0.4-3.7) | 23 | 12.1 (2.3-138.4) | 7.8 (0.6-61.9) | 8.5 (0.9-62.3) |
| 3 | 47 | 1.3 (0.5-3.1) | 46 | 10.7 (1.7-285.7) | 7.3 (0.6-118.2) | 8.3 (1.0-119.0) |
| 4 | 37 | 1.1 (0.5-3.9) | 30 | 11.3 (1.8-1428.0) | 5.1 (0.6-326.8) | 6.1 (0.9-327.0) |
| 5 | 26 | 1.2 (0.6-3.8) | 25 | 12.5 (1.7-4042.6) | 9.0 (0.6-322.9) | 9.2 (1.5-323.0) |
| 6 | 20 | 1.2 (0.6-3.6) | 19 | 14.3 (1.7-907.5) | 10.7 (0.6-205.8) | 11.1 (1.5-206.0) |
| 7 | 11 | 1.3 (0.7-3.5) | 11 | 32.6 (1.8-677.9) | 12.9 (0.9-180.7) | 14.0 (2.0-181.0) |
| 8 or more | 10 | 0.9 (0.5-1.8) | 8 | 19.4 (2.6-107.1) | 12.0 (1.8-32.7) | 13.0 (3.0-33.0) |
| Trend test | P = .025 | P = .35 | –‡ | P = .30 | ||
Individual sample results with an unquantifiable M-protein concentration were excluded from these analyses.
Subjects with a kappa-lambda FLC-ratio less than 0.26 and more than 1.65 were defined as having an “involved lambda” and “involved kappa” FLC, respectively. For persons with an involved lambda FLC, the involved FLC-ratio was computed as the ratio of lambda over kappa. For persons with an involved kappa FLC-ratio, it was computed by dividing kappa with lambda. Similarly, for persons with an involved lambda FLC, the involved-uninvolved FLC concentration was computed by subtracting kappa from lambda; and for persons with an involved kappa FLC, it was computed by subtracting lambda from kappa. All individuals with a kappa-lambda FLC-ratio within the normal range (reference: 0.26-1.65) were excluded from these analyses.
Because the involved-uninvolved FLC concentration (mg/dL) values were not normally distributed even after transformation, the estimated ptrend value (P = .27) was not considered to be reliable.
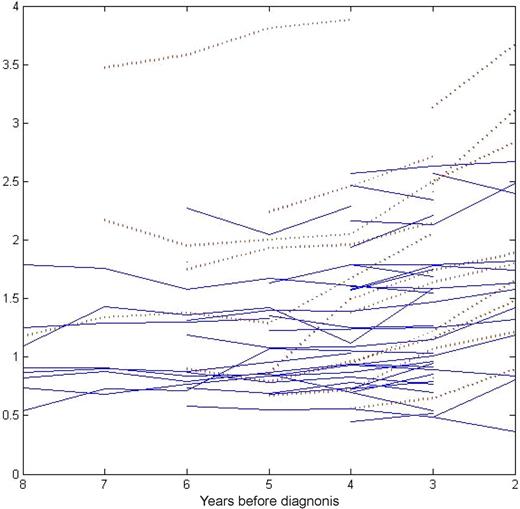
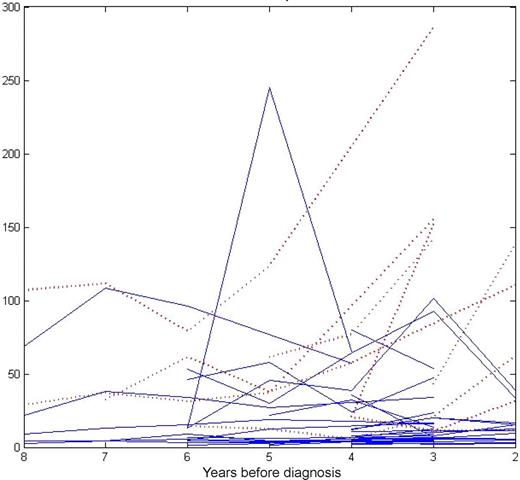
When we evaluated longitudinal M-protein patterns in individual study subjects, in approximately half the study subjects we found evidence of a year-by-year concentration increase prior to MM diagnosis and in the other half the concentration was fairly stable (Figure 1). At 2+ years prior to MM diagnosis, there were 3 subjects with presence of an M-protein concentration greater than 3 g/dL (Figure 1). When we assessed the involved FLC-ratio the same way, we saw the same type of patterns (Figure 2).
M-protein concentration (g/dL) levels year by year prior to multiple myeloma diagnosis.* In approximately half the study population, the M-protein concentration levels showed a year-by-year increase prior to multiple myeloma diagnosis (red dashed line), whereas the other half maintained largely stable abnormal M-protein level up to the diagnosis of multiple myeloma (blue solid line). *Including all subjects with a quantifiable M-protein level.
M-protein concentration (g/dL) levels year by year prior to multiple myeloma diagnosis.* In approximately half the study population, the M-protein concentration levels showed a year-by-year increase prior to multiple myeloma diagnosis (red dashed line), whereas the other half maintained largely stable abnormal M-protein level up to the diagnosis of multiple myeloma (blue solid line). *Including all subjects with a quantifiable M-protein level.
Involved FLC-ratio year by year prior to multiple myeloma diagnosis.* In approximately half the study population, the involved FLC-ratio levels showed a year-by-year increase prior to multiple myeloma diagnosis (red dashed line), whereas the other half did not (blue solid line). *Including all subjects with an abnormal kappa-lambda FLC-ratio. Serum samples with a kappa-lambda FLC-ratio less than 0.26 and more than 1.65 were defined as having an “involved lambda” and “involved kappa” FLC-ratio, respectively. For samples with an involved lambda FLC-ratio, the involved FLC-ratio was computed by diving lambda with kappa. For samples with an involved kappa FLC-ratio, it was computed by dividing kappa with lambda. All samples with a kappa-lambda FLC-ratio within the normal range (reference: 0.26-1.65) were excluded from these analyses.
Involved FLC-ratio year by year prior to multiple myeloma diagnosis.* In approximately half the study population, the involved FLC-ratio levels showed a year-by-year increase prior to multiple myeloma diagnosis (red dashed line), whereas the other half did not (blue solid line). *Including all subjects with an abnormal kappa-lambda FLC-ratio. Serum samples with a kappa-lambda FLC-ratio less than 0.26 and more than 1.65 were defined as having an “involved lambda” and “involved kappa” FLC-ratio, respectively. For samples with an involved lambda FLC-ratio, the involved FLC-ratio was computed by diving lambda with kappa. For samples with an involved kappa FLC-ratio, it was computed by dividing kappa with lambda. All samples with a kappa-lambda FLC-ratio within the normal range (reference: 0.26-1.65) were excluded from these analyses.
Among subjects ever found to have an M-protein prior to MM diagnosis (n = 64; 90.1%), 44 (67.7%), 14 (21.5%), 1 (1.5%), and 2 (3.0%) had an IgG, IgA, IgM, and biclonal isotype, respectively. The serum light chain type was kappa in 39 (60.9%), lambda in 20 (31.3%), and biclonal 2 (3.1%) subjects. There were 3 (4.7%) subjects with a kappa monoclonal light chain but no associated heavy chain. None of the study subjects changed isotype or light chain status over time.
Discussion
Although long-term follow-up data on MGUS patients show an excess risk of developing MM and related malignancies,6,14,15 it is unknown whether MM is typically preceded by MGUS. We hypothesized that a premalignant stage of a protracted length of time always precedes MM. Using the prospective PLCO Cancer Screening Trial,7 we found that virtually all MM cases are preceded by MGUS. This establishes a key role for MGUS in the pathway to MM, of particular relevance for investigations designed to uncover pathogenetic mechanisms in myelomagenesis, for the identification of novel molecular targets, and ultimately for future preventive trials.16 The events that trigger progression of MGUS will be of prime interest. At the same time, however, one has to keep in mind that the vast majority of MGUS cases will never develop MM. Indeed, in a recent study, we found MGUS cases with an abnormal serum kappa-lambda FLC-ratio, non-IgG MGUS, and a high serum M-protein level (> 1.5 g/dL) to have a 58% absolute risk of developing MM at 20 years of follow up, whereas, in sharp contrast, MGUS cases with none of these risk factors had only a 5% absolute risk of MM progression (when accounting for death as a competing risk, the corresponding absolute risk estimates were 27% and 2%, respectively).12 These findings suggest that the well-documented 1% annual average risk of MM progression among MGUS patients6,14,15 is highly heterogeneous and emphasize the fact that the risk of developing MM varies greatly among patients diagnosed with MGUS.12 Taken together, there are emerging needs to integrate serum protein, genetic, and other molecular markers with the overall aim to define subsets of MGUS cases at high versus low risk of developing MM. Our finding that MM is universally preceded by a prolonged premalignant stage with up to 75% of MM patients having detectable M-protein 8 or more years prior to diagnosis of the malignancy fills a key gap in the present literature on myelomagenesis. Important tasks are to develop individualized follow-up and intervention approaches for MGUS patients.17,,–20
Because long-term follow-up studies of MGUS cases have shown that the excess average annual MM risk does not diminish even after 25 to 35 years,6,14 currently, most patients diagnosed with MGUS are typically followed for life by their responsible primary care provider.20 In our study, we found that the median M-protein concentrations increased over time prior to MM. Simultaneously, we found that the proportion of study subjects with an abnormal kappa-lambda FLC-ratio at 8+ to 2 years prior to MM varied between 47% and 85%. This pattern adds substantially to our previous investigation focusing on serum protein abnormalities and subsequent risk for MM. In that study, we found that approximately 30% of all MGUS cases had an abnormal kappa-lambda FLC-ratio, and if the ratio was abnormal, there was a 2.6-fold increase for progression.12 In the present study, when we assessed FLC variations on a group level, year by year in a 10-year interval prior to MM diagnosis, there was no statistical association over time. In accord with recent observations,21 when we evaluated M-protein and involved FLC-ratios over time in individual patients, approximately half the study population showed a year-by-year increase prior to MM diagnosis, whereas the other half maintained largely stable abnormal serum protein level up to the diagnosis of MM. Although it remains to be confirmed, others have speculated that “evolving MGUS” potentially could be a marker for an “early” myeloma with a slow rate of progression.21 Future studies are needed to provide insights to the pathogenesis of MGUS and predictors for MM progression. A better understanding of mechanisms mediating monoclonal plasma-cell proliferation, survival, and migration in the bone marrow microenvironment will improve our insights on myelomagenesis and help us to identify novel molecular targets.22 Larger prospective samples will be required to further refine these patterns.
Strengths of our study include its population-based prospective design, available stored multiple prediagnostic blood samples, and the application of high-quality assays for the determination of prediagnostic protein abnormalities. Our study has some limitations. Because the population-based PLCO cancer screening study enrolled healthy people who were 55 to 74 years at baseline, we were not able to define the prevalence of MGUS prior to a diagnosis of MM among persons diagnosed at younger ages. In addition, due to the PLCO study design, we did not have access to samples (host and tumor material) obtained at the time of MM diagnosis. Neither did we have access to any clinical, laboratory, or pathological details, or death certificates regarding the MM patients. As stated in “Study population, MM patients, and sample handling,” trained PLCO data abstracters reviewed and confirmed all reported cancers. It may also be questioned whether the high frequency of MGUS prior to MM diagnosis represents, in part, undetected MM present prior to the overt manifestations of MM. To minimize the influence of undetected MM in our study, we included only blood samples that were collected 2 or more years prior to MM diagnosis. It is very unlikely for untreated MM patients (ie, those who have undergone a biologic MGUS to MM transformation) to not develop any symptoms that will lead to the diagnosis of the disease over a 2-year period. Thus, regardless of the terminology used (MGUS or otherwise), we can confidently say that the presence of an M-protein in 93% of patients with MM 7 years before diagnosis of MM as seen in this study strongly confirms that a protracted premalignant stage (biologic MGUS) precedes all cases of MM.
In conclusion, based on electrophoresis, immunofixation, and FLC assays, we found that MM is consistently preceded by MGUS. The group median for M-protein concentration exhibited a year-by-year increase over time. Two years prior to MM diagnosis, the proportion of MGUS cases with an abnormal FLC-ratio was 85%, supporting a role for FLC assays in routine MGUS follow up. In approximately half the study population, the M-protein concentration and involved FLC-ratio levels showed a year-by-year increase prior to MM diagnosis, whereas the other half maintained largely stable abnormal serum protein level up to the diagnosis of MM. Thus, stable M-protein or FLC levels do not exclude the development of MM development. Until better molecular markers for progression to MM are available, clinicians have to use clinical measures in combination with routine blood test (including renal function, hemoglobin, and serum calcium) and serum and urine M-protein markers in their monitoring of MGUS cases.20
Future studies are needed to provide new insights on the pathogenesis of MGUS and better predictors for development of MM in order to take early actions to prevent or delay MGUS progression.22
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Drs Christine Berg and Philip Prorok, Division of Cancer Prevention, National Cancer Institute; the Screening Center investigators and staff of the Prostate, Lung, Colorectal, and Ovarian Cancer Screening Trial; Mr Tom Riley and staff, Information Management Services (Rockville, MD); and Ms Barbara O'Brien and staff, Westat (Rockville, MD). Most importantly, we acknowledge the study participants for their contributions to making this study possible.
This research was supported by the Intramural Research Program of the National Cancer Institute, National Institutes of Health (Bethesda, MD); the National Cancer Institute Director's Intramural Innovation Award (O.L.); the grants CA 62242 and CA 107-476-03 from the National Cancer Institute; and the facilities and resources of the Divisions of Hematology, Biostatistics, Clinical Biochemistry and Immunology, and Epidemiology at the Mayo Clinic. The study sponsors did not have any role in the design of the study; the collection, analysis, and interpretation of the data; the writing of the paper; or the decision to submit the paper for publication.
National Institutes of Health
Authorship
Contribution: O.L. and S.V.R. had full access to all the data in the study, had final responsibility for the decision to submit the article for publication, oversaw all aspects of the study, participated in the study conception and design, interpreted the data, drafted the article, managed all revisions to the article, and obtained funding for the study; R.J.C. conducted all the electrophoresis and immunofixation analyses; R.A.K. and J.A.K. reviewed all serum protein electrophoretic patterns; R.M.P. was primarily responsible for the statistical analysis and interpretation of the data and takes responsibility for the accuracy of the data analysis; she also participated in preparation of the article; R.J.C., R.A.K., J.A.K., A.D., S.K., R.H., D.B., and N.E.C. participated in the study design and interpretation of the data, and made important intellectual contributions to the article; all authors read, gave comments, and approved the final version of the article.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ola Landgren, National Cancer Institute, National Institutes of Health, Center for Cancer Research, Medical Oncology Branch, Bldg 10, Room 13N240, 10 Center Dr, Bethesda, MD, 20892; e-mail: landgreo@mail.nih.gov.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal