Abstract
Treatment with the antimalarial drug hydroxychloroquine (HCQ) has been associated with reduced risk of thrombosis in the antiphospholipid (aPL) syndrome (APS) and, in an animal model of APS, with reduction of experimentally induced thrombosis. Recognition of β2-glycoprotein I (β2GPI) by aPL antibodies appears to play a major role in the disease process. We therefore used the techniques of ellipsometry and atomic force microscopy (AFM) to investigate whether HCQ directly affects the formation of aPL IgG–β2GPI complexes on phospholipid bilayers. HCQ, at concentrations of 1 μg/mL and greater, significantly reduced the binding of aPL-β2GPI complexes to phospholipid surfaces and THP-1 (human acute monocytic leukemia cell line) monocytes. The drug also reduced the binding of the individual proteins to bilayers. This HCQ-mediated reduction of binding was completely reversed when the HCQ-protein solutions were dialyzed against buffer. HCQ also caused modest, but statistically significant, reductions of clinical antiphospholipid assays. In conclusion, HCQ reduces the formation of aPL-β2GPI complexes to phospholipid bilayers and cells. This effect appears to be due to reversible interactions between HCQ and the proteins and may contribute to the observed reduction of thrombosis in human and experimental APS. These results support the possibility that HCQ, or analogous molecules, may offer novel nonanticoagulant therapeutic strategies for treating APS.
Introduction
The antiphospholipid (aPL) syndrome (APS) is a thrombophilic disorder that is defined by the presence of autoantibodies against phospholipid-binding cofactor proteins in patients with vascular thrombosis and/or pregnancy complications.1 Of the various phospholipid-binding proteins, aPL antibody recognition of the phospholipid-binding protein, β2-glycoprotein I (β2GPI), appears to particularly correlate with thrombosis2 and is associated with significantly increased risk of thrombosis.3 Antiphospholipid antibodies have been demonstrated to play a causal role in the development of thrombosis in animal models (reviewed in Rand4 ). Long-term anticoagulation with warfarin, a medication that carries a significant risk of bleeding complications,5 is the standard treatment for APS-associated thrombosis.6
Hydroxychloroquine (HCQ), an amphiphilic antimalarial compound, has proven to be an effective immunosuppressive treatment of systemic lupus erythematosus (SLE).7-11 The Hopkins Lupus Cohort reported that the presence of aPL antibodies is an independent predictor of thrombosis in SLE, and that treatment of SLE patients with HCQ was associated with a reduced risk of thrombosis.12 A cross-sectional study that compared aPL antibody–positive patients with thrombosis to a group of patients having the antibodies but who did not have thrombotic histories indicated that HCQ may be protective against thrombosis.13 HCQ significantly reduced the extent of thrombosis in an animal model of injury-induced thrombosis in APS,14 and, in a similar model, also reversed aPL antibody–induced platelet activation.15
Because HCQ has a high protein-binding capacity,16 we asked whether the drug might exert a direct effect on the formation of aPL IgG–β2GPI complexes on phospholipid bilayers. To our knowledge, this question has not been previously addressed. This was investigated with ellipsometry, a technique that allows precise measurement of aPL antibody–β2GPI complexes binding to phospholipid bilayers.17,18 The effects of the drug on the morphologic structure of the protein complexes were observed with atomic force microscopy (AFM).19 We also measured the effect of HCQ on the binding of aPL antibodies to THP-1 monocytes. Finally, to begin to unravel the biochemical basis for the effects, we studied the effects of HCQ on the binding of the individual proteins to phospholipid and the effect of dialysis on binding. HCQ concentrations of 1 μg/mL and greater were used for these experiments because the mean blood concentration of drug in SLE patients who comply with treatment was reported to be in that range.20 We also investigated the effects of HCQ on clinical assays that are used for diagnosis of APS, the anticardiolipin IgG, anti-β2GPI IgG, and the dilute Russell viper venom time (dRVVT).
Methods
Reagents
The study was approved by Montefiore Medical Center Research Administration as project no. 06-10-419E. Informed consent was obtained in accordance with the Declaration of Helsinki. Polyclonal IgG antibody fractions were isolated from citrated plasma of 3 patients with severe APS and 3 healthy control subjects with a protein G column, as described by Sammaritano et al.21 The preparations of aPL antibodies from the patients were compared with IgG preparations obtained from 3 control plasmas. All 3 patients had severe primary APS (ie, there was no evidence of SLE or any other autoimmune disorder) that was manifested by deep vein thrombosis, pulmonary embolism, stroke, and high titers of anticardiolipin (aCL) IgG; one of the patients also had recurrent spontaneous pregnancy losses.
A previously described human monoclonal aPL IgG antibody, designated IS4, that recognizes β2GPI and anionic phospholipid,22 was used for AFM imaging of the effects of HCQ on the immune complexes. The monoclonal antibody (mAb) was selected because it is a highly specific and purified reagent, qualities necessary for high resolution of AFM imaging, and because it has been well characterized. IS4 recognizes β2GPI and does not have lupus anticoagulant activity by dilute Russell viper venom time or kaolin clotting time.22-24 The mAb is thrombogenic in animal model systems,25 binds to cultured human umbilical vein endothelial cells, and induces leukocyte adhesion to murine endothelium in venules of the microcirculation.25,26 It has also been shown by AFM to disrupt the crystallization of annexin A5 and to blunt its anticoagulant activity.19 The aPL mAb was generated from the peripheral blood mononuclear cells of a patient with APS and was purified by affinity columns as previously described.22 A commercially available non–immune human IgG derived from patients with monoclonal gammopathies (Sigma-Aldrich, St Louis, MO) was used as a control.
Human β2GPI was purchased from Intracel (Frederick, MD). Purity of the protein was confirmed by SDS–polyacrylamide gel electrophoresis (PAGE) and Western blot, which showed single band at 50 kDa. A stock solution of HCQ (kind gift from Dr Kirk Sperber of Mount Sinai School of Medicine) was made up with HEPES-buffered saline (HBS) consisting of 0.01 M HEPES, 0.14 M NaCl, pH 7.5, at 200 mg/mL and stored at 4°C. The pH measurements of HCQ, diluted in HBS at the concentration of 1 μg/mL and 1 mg/mL—the lowest and highest concentrations used for current studies—were 7.45.
Ellipsometry studies
The effects of HCQ on the binding of the proteins to phospholipid bilayers were studied using ellipsometry, as previously described.18,27 All experiments were performed at room temperature in duplicate to confirm the results. Briefly, phospholipid bilayer (50 μM) composed of 30% 1,2-dioleoyl-sn-glycero-3-phospho-L-serine (PS) and 70% 1,2-dioleoyl-sn-glycero-3-phosphocholine (PC; Avanti Polar-lipids, Alabaster, AL) was formed on reflective silicon slides, as previously described.19 The mounted bilayers were transferred to an ellipsometry cuvette containing 1 mL stirring buffer composed of 0.01 M HEPES, 0.14 M NaCl 0.05%, bovine serum albumin, and 1.25 mM calcium (HBSA, pH 7.5).
To investigate the effects of HCQ on phospholipid-bound immune complexes, a mixture of aPL or control IgG (0.5 mg/mL) and β2GPI (5 μg/mL) was added to the bilayer, and the binding of the proteins was monitored with a thin film ellipsometer (Rudolph & Sons, Fairfield, NJ). After the protein adsorption had reached equilibrium, increasing concentrations of HCQ (0, 0.001, 0.01, 0.1, 0.2, 0.5, and 1 mg/mL) were serially added, and the effects of HCQ on the phospholipid-bound complexes were measured. Pilot studies indicated that 1 μg/mL HCQ had a progressive effect on desorbing complexes from the bilayers over the course of approximately 4 hours. For the present studies, mixtures of aPL, versus control IgG (final concentration 0.5 mg/mL), and β2GPI (5 μg/mL) were incubated with HCQ (1 μg/mL) in HBS or buffer alone (control) overnight at 4°C. The IgG-β2GPI-HCQ mixture was then added to the HBSA and the effects of HCQ on the phospholipid-bound complexes were determined. Experiments were also performed with IS4 (0.1 mg/mL), the aPL mAb used for AFM imaging studies described in the next section, to determine whether the mAb would also bind to the phospholipid bilayer, and whether HCQ would dissociate the bound complexes from the bilayer. In addition to investigating the effects of HCQ on the phospholipid-bound complexes, we also investigated the effects of HCQ (1 mg/mL) separately on the phospholipid-bound β2GPI and on phospholipid-bound aPL IgG. Polyclonal aPL IgG alone (0.5 mg/mL), or β2GPI (5 μg/mL) alone, was added to the bilayers in HBSA. HCQ (1 mg/mL) was added after the protein adsorption monitored by ellipsometry had reached equilibrium, and HCQ-induced dissociation of the protein from the bilayer was measured.
To measure the ability of HCQ to inhibit the binding of β2GPI and aPL IgG mAb (IS4) to phospholipid bilayers, we determined binding isotherms for each protein, both in the presence and absence of HCQ. The aPL mAb was used for this purpose because the aPL IgG derived from blood is composed of heterogeneous proteins. Briefly, HCQ (1 mg/mL) or buffer control was added to the cuvette containing the phospholipid bilayer, and then aliquots of β2GPI (up to 10 μg/mL) or aPL mAb (up to 0.1 mg/mL) were serially added, allowing each addition to reach equilibrium before subsequent additions. Based on the measured surface density of bound protein and the total amount of protein added to the cuvette, traditional graphs of phospholipid-bound versus free protein were generated. Using SigmaPlot software (SPSS, Chicago, IL), Langmuir isotherms were fit simultaneously to binding data, both with and without HCQ, to determine a Kd in the absence of HCQ, a Kd in the presence of 1 mg/mL HCQ, and a maximum binding capacity that is independent of HCQ.
We then investigated whether the effect of HCQ might be due to a direct interaction of the drug with the phospholipid bilayer, rather than with the proteins. HCQ (1 mg/mL) was added to the cuvette containing the phospholipid bilayer and, after 15 minutes, flushed away with 30 mL HBSA. A mixture of aPL IgG (0.5 mg/mL) and β2GPI (5 μg/mL) was then added to the HCQ-treated bilayer and the protein binding was monitored by ellipsometry. The effect of dialysis on the HCQ-mediated reduction of complex binding was also studied to determine whether the action of HCQ was sustained or reversible. Mixtures of aPL IgG (0.5 mg/mL) and β2GPI (5 μg/mL) were incubated with HCQ (at 1 μg/mL and 1 mg/mL) or buffer control overnight at 4°C. The preparations were then thoroughly dialyzed against HBS before addition to the bilayers in HBSA. Binding of the proteins was monitored by ellipsometry.
Imaging studies
The effects of HCQ on the binding of β2GPI and aPL mAb to phospholipid bilayers were also visualized with dynamic AFM imaging experiments, performed as previously described.19 Briefly, planar phospholipid bilayers (50 μM; 30% PS and 70% PC) were formed on freshly cleaved 1.2-cm mica discs (Ashville-Schoonmaker Mica, Newport News, VA). β2GPI (final concentration approximately 10 μg/mL) was then added to HBS (the same buffer as used for the ellipsometry studies, but lacking BSA) covering the bilayers and incubated overnight at 4°C. The following morning, the binding of β2GPI to the phospholipid bilayer was observed using “tapping mode” imaging in buffer with a Digital Instruments BioScope (Nanoscope IIIa controller; Veeco, Santa Barbara, CA) using oxide-sharpened silicon nitride pyramidal probes (Advanced Surface Microscopy, Indianapolis, IN). aPL mAb IS4 (20 μg/mL) was then added to the preparation, and antibody-cofactor complexes were observed with continuous imaging to have formed within 30 minutes over the bilayer. After 100 minutes of imaging, HCQ (1 mg/mL) was added to the fluid covering the bilayer and the preparation was continuously imaged with the AFM for up to 1 hour. Quantitative analysis of the effects of HCQ on the phospholipid-bound aPL mAb–β2GPI complexes was performed by height measurement—which represents the thickness of the immune complexes—of randomly encountered immune complexes before the addition of HCQ and at 12 minutes and 30 minutes after addition.
THP-1 cell cultures
THP-1, a human monocyte cell line derived from a patient with monocytic leukemia, was obtained from the ATCC (Rockville, MD). The cells were maintained in complete growth medium (CGM) composed of ATCC-formulated RMPI-1640 medium, 10% fetal bovine serum (ATCC), and 0.05 mM 2-mercaptoethanol at 37°C in a CO2 incubator (Isotemp; Fisher Scientific, Pittsburgh, PA) containing 5% carbon dioxide and 95% air, as described by ATCC. To determine the effects of HCQ on the binding of aPL IgGs to the cell membrane, the cells were resuspended to a density of 3.6 × 105 cells/mL in medium consisting of 80% CGM and 20% aPL and control IgGs (0.2 mg/mL) in HBS (pH 7.45), with or without HCQ added (at 1 μg/mL and 1 mg/ML). The cells were then aliquoted into 24-well culture plates (1 mL/well) and maintained for 18 hours in the incubator. The cells were transferred to Eppendorf tubes and centrifuged for 8 minutes at 250g at 20°C with a microcentrifuge (Eppendorf Centrifuge 5417R; Brimkman Instruments, Westbury, NY). The supernatants were removed, the cells were washed once with HBS (1 mL) and then centrifuged again. The cells were incubated with HRP-conjugated antihuman IgG (50 μL) for 15 minutes at room temperature, washed twice with HBS, and then incubated with TMB substrate (50 μL) for 10 minutes at room temperature, at which time, sulfuric acid (0.36 N; 50 μL) was added. The cells were centrifuged for 10 minutes at 10 000g at 20°C, after which the supernatants were transferred to a 96-well microtiter plate. The optical absorbance was measured at 450 nm with a reference wavelength of 650 nm. Results were read against a standard curve using cardiolipin-coated microtiter plates and, because all assays had been performed with the same cell suspension, were reported as arbitrary aCL IgG units per well (AU/well). All studies were done with duplicate culture wells. The cell density/well was 4 × 105 after an 18-hour incubation. Trypan blue exclusion studies showed that the treated cells were at least 97% viable.
Anticardiolipin IgG enzyme-linked immunosorbent assay
The effects of HCQ on aCL IgG binding were determined using a commercially available anticardiolipin IgG antibody immunoassay (REAADS Medical Products, Westminster, CO). Excess serum samples from 30 samples with aCL IgG levels of more than 23 GPL units used for clinical assays were deidentified and collected; the samples were incubated with HCQ, at 1 μg/mL and 1 mg/mL, or buffer control overnight at 4°C. They were then diluted in sample diluent containing the same concentrations of HCQ or buffer control and assayed for aCL IgG according to the manufacturer's instruction.
Anti-β2GPI IgG enzyme-linked immunosorbent assay
We investigated the effects of HCQ on antibody binding to β2GPI binding as previously described,28 with minor modifications. Briefly, microtiter plates (MaxiSorp Surface, Nunc-Immuno plate; Fisher Scientific) were coated with β2GPI (10 μg/mL) in 50 mM carbonate buffer (15 mM Na2CO3, 35 mM NaHCO3, pH 9.6) overnight at 4°C. The plates were blocked with blocking buffer (PBS with 1% BSA, pH 7.4) for 60 minutes and washed with PBS containing 0.1% Tween. Excess sera from 15 samples with elevated anti-β2GPI IgG levels used for clinical assays were deidentified and collected. The samples were incubated with HCQ, at 1 μg/mL and 1 mg/mL, or buffer control overnight at 4°C. They were then diluted (1:50) in HBS containing 1% BSA, 0.1% Tween, and the same concentrations of HCQ or buffer control and incubated in the β2GPI-coated plates for 120 minutes at room temperature. The plates were then washed 4 times with PBS-Tween and incubated with goat anti–human HRP-conjugated IgG (REAADS Medical Products) for 30 minutes; the plates were then washed again and incubated with TMB substrate (REAADS Medical Products) for 10 minutes at room temperature. The enzymatic reaction was stopped by sulfuric acid (0.36 N). The optical absorbance of each well was measured at 450 nm with a reference wavelength of 650 nm using a microtiter-plate reader (SPECTRAmax Plus 384; Molecular Devices, Sunnyvale, CA).
Lupus anticoagulant test
Ten deidentified excess plasmas with elevated lupus anticoagulant (LA) ratios were collected from samples used for clinical assays. The plasmas were incubated with HCQ, at 1 μg/mL and 1 mg/mL, or buffer control overnight at 4°C. The samples were sent to the Montefiore Medical Center Advanced Coagulation Laboratory where standard clinical LA tests were performed by dilute Russell viper venom times using a commercially available kit (Life Diagnostics, Life Therapeutics, Clarkston, GA) on an automated Behring Coagulation System (Dade Behring, Deerfield, IL). In accordance with the manufacturer's instructions, the assays were performed in duplicate in the absence and presence of excess phospholipid (Confirm reagent) provided in the kits. The results were expressed as LA ratios of the mean clotting times obtained in the absence of excess phospholipid divided by the mean clotting times obtained in the presence of excess phospholipid, in accordance with the manufacturer's instructions.
Statistical analysis
Measurements of protein binding in the presence and absence of HCQ, including adsorption measurements performed by ellipsometry, aCL IgG, and anti-β2GPI enzyme-linked immunosorbent assays (ELISAs), lupus anticoagulant activity and height analyses of the complexes were compared using paired 2-tailed t test (Instat program; GraphPad, San Diego, CA). P values less than .05 were considered statistically significant.
Results
Ellipsometry studies
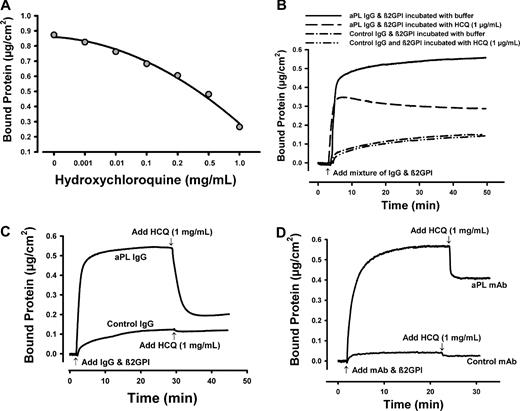
Addition of increasing concentrations of HCQ to phospholipid-bound aPL IgG–β2GPI complexes resulted in a progressive dose-related desorption of the complexes from the bilayer between 0 and 1 mg/mL HCQ (Figure 1A). As mentioned in “Ellipsometry studies,” pilot studies investigating the effect of incubation time using the lowest concentration of HCQ, 1 μg/mL, on aPL IgG and β2GPI complex binding indicated that the effect was progressive over time and reached maximum at approximately 4 hours. We therefore preincubated mixtures of aPL IgG and β2GPI with 1 μg/mL HCQ overnight at 4°C before addition to the bilayer. There was significant reduction of the binding of the immune complexes preincubated with 1 μg/mL HCQ (mean ± SD: 0.29 ± 0.10 μg/cm2, compared with 0.57 ± 0.07 μg/cm2 for the complexes incubated with buffer controls; n = 3 different aPL IgGs; P = .003; Figure 1B). The mean (± SD) of HCQ-induced reduction of immune complex binding was 50% plus or minus 31% (range, 38%-61%). At a HCQ concentration of 1 mg/mL, preincubation with the proteins was not required to see its effect. Addition of HCQ at 1 mg/mL to phospholipid-bound complexes resulted in the immediate dissociation of complexes from the bilayers (Figure 1C); the same concentration of HCQ had no effect on the adsorption of control IgG and β2GPI (Figure 1C). Similarly, the aPL IgG mAb (IS4), used for AFM imaging studies described in the next section, formed immune complexes on phospholipid bilayers whose adsorption was also immediately reversed by addition of 1 mg/mL HCQ (Figure 1D). There was no significant effect of the drug on the adsorption of the control mAb and β2GPI.
Ellipsometry studies of the effect of HCQ on binding of aPL IgG and β2GPI complexes to phospholipid bilayers (30% PS/70% PC). (A) Effects of various concentrations of HCQ on the protein binding. A mixture of aPL IgG (0.5 mg/mL) and β2GPI (5 μg/mL) in HBSA was added to phospholipid bilayer. After the adsorption of the protein had reached equilibrium, increasing doses of HCQ (0.001, 0.01, 0.1, 0.2, 0.5, and 1 mg/mL) were serially added. There was a progressive dose-related dissociation of the complexes from the phospholipid bilayers. Each point shows the mean of duplicate experiments. (B) Ellipsometry tracing of aPL IgG (0.5 mg/mL) premixed with β2GPI (5 μg/mL) and incubated with HCQ (1μg/mL) or control buffer overnight at 4°C before addition to the bilayers. The HCQ-treated immune complexes showed reduced binding compared with the buffer-treated complexes. HCQ had no effect on the adsorption of control IgG and β2GPI. (C) Immediate dissociation of phospholipid-bound aPL IgG–β2GPI complexes by HCQ (1 mg/mL). The drug had no significant effect on the adsorption of control IgG and β2GPI. (D) Similar ellipsometry study with the aPL IgG mAb (IS4) and β2GPI. The phospholipid-bound proteins were rapidly dissociated from the phospholipid bilayer by HCQ (1 mg/mL). There was no significant effect of the drug on the adsorption of control mAb and β2GPI.
Ellipsometry studies of the effect of HCQ on binding of aPL IgG and β2GPI complexes to phospholipid bilayers (30% PS/70% PC). (A) Effects of various concentrations of HCQ on the protein binding. A mixture of aPL IgG (0.5 mg/mL) and β2GPI (5 μg/mL) in HBSA was added to phospholipid bilayer. After the adsorption of the protein had reached equilibrium, increasing doses of HCQ (0.001, 0.01, 0.1, 0.2, 0.5, and 1 mg/mL) were serially added. There was a progressive dose-related dissociation of the complexes from the phospholipid bilayers. Each point shows the mean of duplicate experiments. (B) Ellipsometry tracing of aPL IgG (0.5 mg/mL) premixed with β2GPI (5 μg/mL) and incubated with HCQ (1μg/mL) or control buffer overnight at 4°C before addition to the bilayers. The HCQ-treated immune complexes showed reduced binding compared with the buffer-treated complexes. HCQ had no effect on the adsorption of control IgG and β2GPI. (C) Immediate dissociation of phospholipid-bound aPL IgG–β2GPI complexes by HCQ (1 mg/mL). The drug had no significant effect on the adsorption of control IgG and β2GPI. (D) Similar ellipsometry study with the aPL IgG mAb (IS4) and β2GPI. The phospholipid-bound proteins were rapidly dissociated from the phospholipid bilayer by HCQ (1 mg/mL). There was no significant effect of the drug on the adsorption of control mAb and β2GPI.
Atomic force microscopy imaging studies
AFM imaging of phospholipid-coated mica disks revealed that the addition of β2GPI resulted in the formation of distinct structures raised above the phospholipid bilayer (Figure 2A,E,I), similar to those that have been previously described.29 On addition of aPL mAb IS4, large aggregates of increased height composed of aPL mAb–β2GPI complexes over the bilayer were observed (Figure 2B,F,J). At 12 minutes after the addition of HCQ (1 mg/mL) to the supernatant fluid, significant disintegration of the complexes was evident (Figure 2C,G,K). At 30 minutes after the addition of HCQ to the fluid, the complexes were further dissipated (Figure 2D,H,L). Quantitative analysis of corresponding height images of the aPL mAb–β2GPI complexes and the aPL mAb–β2GPI complexes at 12 minutes after the addition of HCQ (1 mg/mL) showed reductions of the maximal height of the immune complexes from a mean of 17.7 (± 5.8) nm to 9.3 (± 2.4) nm (n = 40 complex patches; P < .001; Figure 2M).
Atomic force microscopy (AFM) height images (3-dimensional view with 50° pitch) showing the effect of HCQ on aPL mAb and β2GPI complexes on 3 separate complexes. (A,E,I) The binding of β2GPI to phospholipid bilayers. Addition of β2GPI (10 μg/mL) to buffer covering the phospholipid bilayers resulted in the formation of distinct structures raised above the bilayers. (B,F,J) The binding of aPL IgG mAb, IS4, to β2GPI prebound to phospholipids. Addition of aPL mAb (20 μg/mL) to the phospholipid-bound β2GPI shown in panels A, E, and I resulted in large aggregates of increased height (indicated by white color) composed of aPL mAb–β2GPI complexes over the bilayers. (C,G,K) The effect of HCQ at 1 mg/mL on the phospholipid-bound aPL mAb and β2GPI complexes. At 12 minutes after the addition of HCQ to the supernatant fluid covering the bilayer, the immune complexes, shown in panels B, F and J, were significantly eroded after addition of the drug. (D,H,L) The immune complexes, shown in panels B, F, and J, were further disintegrated at thirty minutes after the addition of HCQ (1 mg/mL). All images show complexes electronically zoomed from an original 30 μm × 30 μm scan. Images were minimally processed to remove scan lines. The color shades represent height variations in the images, with the darker colors (rust) indicating lower heights and the lighter colors (white), the higher profiles. (M) Quantitative analysis of the effects of HCQ on 40 randomly encountered aPL mAb–β2GPI complexes. The height of the immune complexes at 12 minutes after the addition of HCQ (1 mg/mL) was significantly decreased (17.7 ± 5.8 nm; vs 9.3 ± 2.4 nm for the height before addition of HCQ).
Atomic force microscopy (AFM) height images (3-dimensional view with 50° pitch) showing the effect of HCQ on aPL mAb and β2GPI complexes on 3 separate complexes. (A,E,I) The binding of β2GPI to phospholipid bilayers. Addition of β2GPI (10 μg/mL) to buffer covering the phospholipid bilayers resulted in the formation of distinct structures raised above the bilayers. (B,F,J) The binding of aPL IgG mAb, IS4, to β2GPI prebound to phospholipids. Addition of aPL mAb (20 μg/mL) to the phospholipid-bound β2GPI shown in panels A, E, and I resulted in large aggregates of increased height (indicated by white color) composed of aPL mAb–β2GPI complexes over the bilayers. (C,G,K) The effect of HCQ at 1 mg/mL on the phospholipid-bound aPL mAb and β2GPI complexes. At 12 minutes after the addition of HCQ to the supernatant fluid covering the bilayer, the immune complexes, shown in panels B, F and J, were significantly eroded after addition of the drug. (D,H,L) The immune complexes, shown in panels B, F, and J, were further disintegrated at thirty minutes after the addition of HCQ (1 mg/mL). All images show complexes electronically zoomed from an original 30 μm × 30 μm scan. Images were minimally processed to remove scan lines. The color shades represent height variations in the images, with the darker colors (rust) indicating lower heights and the lighter colors (white), the higher profiles. (M) Quantitative analysis of the effects of HCQ on 40 randomly encountered aPL mAb–β2GPI complexes. The height of the immune complexes at 12 minutes after the addition of HCQ (1 mg/mL) was significantly decreased (17.7 ± 5.8 nm; vs 9.3 ± 2.4 nm for the height before addition of HCQ).
THP-1 cell line cultures
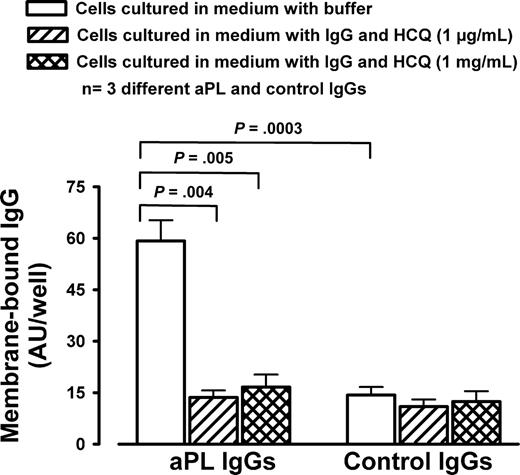
Incubation of THP-1 monocytes with human aPL IgG fractions resulted in significantly greater binding of IgG than incubation with control IgG (59.2 ± 6.0 AU/well vs 14.3 ± 2.3 AU/well; P = .001; Figure 3). The presence of HCQ at concentrations of 1 μg/mL and 1 mg/mL significantly reduced the binding of aPL IgG (13.6 ± 2.0 AU/well for HCQ at 1 μg/mL and 16.6 ± 3.6 AU/well for HCQ at 1 mg/mL, compared with 59.2 ± 0.6 AU/well for the cells incubated with aPL IgG alone; P = .004 and P = .005, respectively) to a level similar to cells incubated with control IgG (Figure 3). HCQ had no effect on the binding of control IgG to THP-1 cells (Figure 3).
Effects of HCQ on aPL IgGs binding to THP-1 monocytes. Incubation of THP-1 monocytes with aPL IgGs resulted in significantly greater IgG binding than incubation with control IgGs. HCQ at both 1 μg/mL and 1 mg/mL significantly reduced the binding of aPL IgGs to levels similar to cells incubated with control IgG. The drug had no effect on the binding of control IgGs to the cells. Error bars represent SD.
Effects of HCQ on aPL IgGs binding to THP-1 monocytes. Incubation of THP-1 monocytes with aPL IgGs resulted in significantly greater IgG binding than incubation with control IgGs. HCQ at both 1 μg/mL and 1 mg/mL significantly reduced the binding of aPL IgGs to levels similar to cells incubated with control IgG. The drug had no effect on the binding of control IgGs to the cells. Error bars represent SD.
Studies of HCQ interaction with proteins
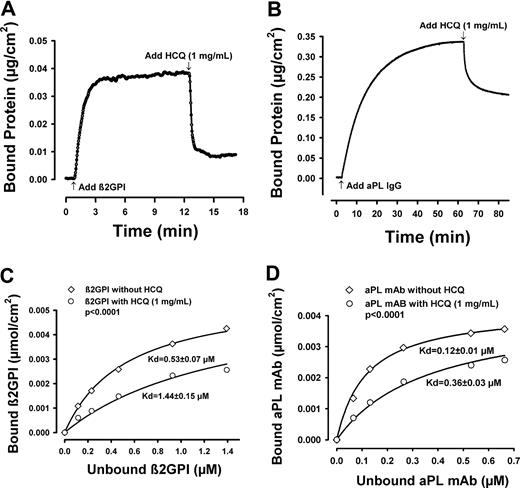
HCQ, at 1 mg/mL, dissociated phospholipid-bound β2GPI (Figure 4A), and also phospholipid-bound polyclonal aPL IgG (Figure 4B), individually from the bilayer. Determination of binding isotherms of β2GPI and aPL IgG mAb to phospholipid bilayer showed that the maximum binding density of β2GPI alone and aPL IgG alone was 0.0057 (± 0.0003) μmol/cm2 (P < .001) and 0.0042 (± 0.0001) μmol/cm2 (P < .001), respectively. In the presence of HCQ (1 mg/mL), the bindings of both β2GPI and aPL mAb were consistently decreased (Figure 4C,D). The drug significantly increased the Kd for β2GPI-phospholipid interactions (1.44 ± 0.15 μM, compared with 0.53 ± 0.07 μM for the Kd in the absence of HCQ; P < .001; Figure 4C) and the Kd for aPL mAb-phospholipid interactions (0.12 ± 0.01 μM, compared with 0.07 ± 0.01 μM for the Kd in the absence of HCQ; P < .001). The results indicate that HCQ decreases the affinity of both aPL mAb and β2GPI for binding to phospholipids.
Studies of HCQ interaction with proteins by ellipsometry. (A) Ellipsometry tracing showing β2GPI (5 μg/mL) binding to phospholipid bilayer and the effect of HCQ (1 mg/mL) on the phospholipid-bound protein. The phospholipid-bound β2GPI was rapidly dissociated from the bilayer by the addition of drug. (B) Ellipsometry tracing showing polyclonal aPL IgG (0.5 mg/mL) binding to phospholipid bilayer and the effects of HCQ at 1 mg/mL on the phospholipid-bound protein. The phospholipid-bound aPL IgG was also readily dissociated from the bilayer by the addition of drug. (C) Binding isotherm of β2GPI to the phospholipid bilayer. In the presence of HCQ (1 mg/mL), the binding of β2GPI was significantly reduced and the Kd was significantly increased compared with the buffer control (1.44 ± 0.15 μM vs 0.53 ± 0.07 μM; P < .001). (D) Binding isotherm of aPL mAb, IS4, in HBSA to phospholipid bilayer. In the presence of HCQ (1 mg/mL), the binding of aPL mAb was significantly reduced and the Kd was significantly increased compared with the buffer controls (0.36 ± 0.03 μM vs 0.12 ± 0.01 μM; P < .001).
Studies of HCQ interaction with proteins by ellipsometry. (A) Ellipsometry tracing showing β2GPI (5 μg/mL) binding to phospholipid bilayer and the effect of HCQ (1 mg/mL) on the phospholipid-bound protein. The phospholipid-bound β2GPI was rapidly dissociated from the bilayer by the addition of drug. (B) Ellipsometry tracing showing polyclonal aPL IgG (0.5 mg/mL) binding to phospholipid bilayer and the effects of HCQ at 1 mg/mL on the phospholipid-bound protein. The phospholipid-bound aPL IgG was also readily dissociated from the bilayer by the addition of drug. (C) Binding isotherm of β2GPI to the phospholipid bilayer. In the presence of HCQ (1 mg/mL), the binding of β2GPI was significantly reduced and the Kd was significantly increased compared with the buffer control (1.44 ± 0.15 μM vs 0.53 ± 0.07 μM; P < .001). (D) Binding isotherm of aPL mAb, IS4, in HBSA to phospholipid bilayer. In the presence of HCQ (1 mg/mL), the binding of aPL mAb was significantly reduced and the Kd was significantly increased compared with the buffer controls (0.36 ± 0.03 μM vs 0.12 ± 0.01 μM; P < .001).
Pretreatment of the phospholipid bilayer alone with HCQ, followed by flushing with HBSA before the addition of the proteins, did not affect the binding of aPL IgG–β2GPI complexes (maximum binding up to 0.505 μg/cm2, compared with 0.507 cm2 for the complexes binding to untreated bilayer). We then studied whether dialysis of HCQ-protein mixtures attenuates or reverses the inhibitory action of HCQ. Incubation of aPL IgG–β2GPI with HCQ (1 μg/mL), without dialysis, significantly reduced the binding of aPL IgG–β2GPI (mean ± SD of 2 experiments: 0.47 ± 0.03 μg/cm2, compared with 0.58 ± 0.01 μg/cm2 for aPL IgG–β2GPI incubated with buffer control without dialysis; P = .04). Dialysis of the mixture that had been incubated with HCQ (1 μg/mL) against buffer restored the binding of the complexes to phospholipids (0.57 ± 0.01 μg/cm2, compared with 0.58 ± 0.01 μg/cm2 without dialysis; P = .42; Figure 5A). Similar results were obtained with dialysis experiments performed with HCQ at concentration of 1 mg/mL (Figure 5B).
Effects of dialysis on the HCQ-mediated reduction of aPL IgG–β2GPI complex binding. Mixtures of aPL IgG (0.5 mg/mL) and β2GPI (5 μg/mL) were incubated overnight with the 2 concentrations of HCQ or control buffer, and the proteins were then dialyzed against buffer before exposure to the bilayers. (A) Incubation of aPL IgG–β2GPI with HCQ at 1 μg/mL, without dialysis, significantly reduced the complex binding; dialysis of the mixture incubated with HCQ (1 μg/mL) against buffer restored the binding of the complexes to phospholipid. (B) Similar results with HCQ at the higher concentration of 1 mg/mL.
Effects of dialysis on the HCQ-mediated reduction of aPL IgG–β2GPI complex binding. Mixtures of aPL IgG (0.5 mg/mL) and β2GPI (5 μg/mL) were incubated overnight with the 2 concentrations of HCQ or control buffer, and the proteins were then dialyzed against buffer before exposure to the bilayers. (A) Incubation of aPL IgG–β2GPI with HCQ at 1 μg/mL, without dialysis, significantly reduced the complex binding; dialysis of the mixture incubated with HCQ (1 μg/mL) against buffer restored the binding of the complexes to phospholipid. (B) Similar results with HCQ at the higher concentration of 1 mg/mL.
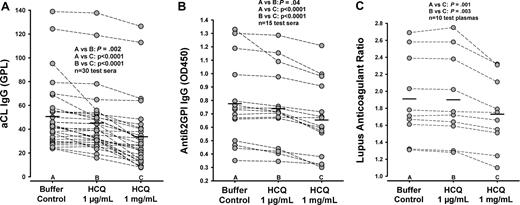
aCL ELISA
Incubation of sera with elevated aCL IgG with HCQ significantly decreased the measured levels of aCL IgG (mean ± SD: 45.2 ± 26.6 GPL for 1 μg/mL HCQ incubation and 33.6 ±28.0 GPL for 1 mg/mL HCQ incubation, compared with 50.6 ± 27.8 GPL for buffer control; n = 30; P = .002 and P < .001, respectively; Figure 6A). The samples incubated with the higher concentration of 1 mg/mL HCQ also had significantly decreased levels of aCL IgG (33.6 ± 28.0 GPL) compared with the samples incubated with HCQ at 1 μg/mL (45.2 ± 26.6 GPL; P < .001; Figure 6A). With 1 μg/mL HCQ, 8 of 30 sera showed decreased aCL IgG levels ranging between 22% and 41%, 6 sera showed no reaction to the drug, and the remainder showed intermediate decreases. With 1 mg/mL HCQ, 21 of 30 sera had decreased aCL IgG levels ranging between 24% to 82%, and the remaining 9 sera showed decreased IgG levels by 2% to 17%.
Effect of HCQ on aCL and anti-β2GPI IgG ELISAs and the LA test. Serum or plasma samples were incubated with HCQ at 1 μg/mL and 1 mg/mL or buffer control overnight at 4°C before the assays. (A) The results of aCL IgG ELISA for sera with elevated aCL IgG levels. Incubation of sera with HCQ significantly decreased the levels of aCL IgG compared with buffer control. The higher HCQ concentration of 1 mg/mL had a greater effect than the lower concentration of the drug. (B) The results of HCQ on anti-β2GPI IgG ELISA. Incubation of sera with HCQ significantly decreased the binding of anti-β2GPI IgG compared with incubation with buffer control. The higher HCQ concentration of 1 mg/mL had a greater effect than the lower concentration of the drug. (C) The results of lupus anticoagulant test for LA-positive plasmas. Incubation of plasmas with HCQ at 1 mg/mL significantly decreased lupus anticoagulant activity compared with the buffer controls and lower concentration of the drug; incubation of plasmas with HCQ at 1 μg/mL showed no significant effect.
Effect of HCQ on aCL and anti-β2GPI IgG ELISAs and the LA test. Serum or plasma samples were incubated with HCQ at 1 μg/mL and 1 mg/mL or buffer control overnight at 4°C before the assays. (A) The results of aCL IgG ELISA for sera with elevated aCL IgG levels. Incubation of sera with HCQ significantly decreased the levels of aCL IgG compared with buffer control. The higher HCQ concentration of 1 mg/mL had a greater effect than the lower concentration of the drug. (B) The results of HCQ on anti-β2GPI IgG ELISA. Incubation of sera with HCQ significantly decreased the binding of anti-β2GPI IgG compared with incubation with buffer control. The higher HCQ concentration of 1 mg/mL had a greater effect than the lower concentration of the drug. (C) The results of lupus anticoagulant test for LA-positive plasmas. Incubation of plasmas with HCQ at 1 mg/mL significantly decreased lupus anticoagulant activity compared with the buffer controls and lower concentration of the drug; incubation of plasmas with HCQ at 1 μg/mL showed no significant effect.
Anti-β2GPI ELISA
Incubation of sera with elevated anti-β2GPI IgG with HCQ resulted in modest, but statistically significant, decreased binding of anti-β2GPI IgG levels (optical density: 0.739 ± 0.283 for 1 μg/mL HCQ incubation and 0.654 ± 0.273 for 1 mg/mL HCQ, compared with 0.775 ± 0.304 for buffer control; n = 15; P = .04 and P < .001, respectively; Figure 6B). Incubation of the samples with HCQ at the higher concentration of 1 mg/mL significantly decreased the levels of anti-β2GPI IgG (0.654 ± 0.273) compared with the samples incubated with HCQ at 1 μg/mL (0.739 ± 0.283; P < .001; Figure 6B).
Lupus anticoagulant test
Incubation of LA-positive plasmas with HCQ at 1 mg/mL significantly decreased lupus anticoagulant activity (LA ratio: 1.49 ± 0.33, compared with 1.91 ± 0.49 for buffer control; n = 10; P = .001; Figure 6C), whereas HCQ at 1 μg/mL showed no effect. Incubation of the samples with HCQ at the higher concentration of 1 mg/mL significantly decreased LA ratios (1.49 ± 0.33) compared with the samples incubated with HCQ at 1 μg/mL (1.90 ± 0.51; P = .003; Figure 6C). With 1 mg/mL HCQ, 6 of 10 plasmas had decreased LA activity by 4% to 13% and 4 plasmas showed no change with the drug.
Discussion
HCQ is an amphiphilic antimalarial molecule that is widely used for nonsteroidal immunosuppressive treatment of SLE and rheumatoid arthritis. Several mechanisms have been proposed to explain this beneficial effect. Among them are the reduction of proteolysis and antigen presentation due to the drug's lysosomotrophic properties and increase of lysosomal pH,30 the inhibition of T-cell receptor– and B-cell antigen receptor–induced calcium signaling,31 and the inhibition of TOLL-like receptor signaling.32 To our knowledge, the possibility that HCQ may directly interfere with binding of aPL antibody–β2GPI to phospholipids has not been previously been addressed.
As mentioned in “Introduction,” a concentration of HCQ of 1 μg/mL and greater was used in this study because that was reported to be the mean blood concentration of drug in SLE patients who comply with treatment.20 The actual concentration of the drug at membranes and organelles where it is bound is not known and may possibly be higher. HCQ is sequestered in a storage compartment, as demonstrated by the prolonged terminal elimination half-life in healthy volunteers of more than 40 days, and the fact that a treatment period of 6 months is required to achieve steady-state levels.33 These properties make it difficult to determine the concentration of drug that is required for therapeutic effectiveness in the microenvironment where its activities are exerted.
The results of these studies clearly demonstrated that HCQ reduced the binding of aPL IgG–β2GPI complexes to phospholipid bilayers. This was demonstrated with quantitative ellipsometry, and confirmed morphologically by atomic force microscopy. HCQ also reduced the binding of aPL IgG to THP-1 monocytes. Structural studies such as x-ray crystallography and nuclear magnetic resonance (NMR) spectroscopy, which are beyond the scope of this initial report, will be required for definitive understanding of how HCQ inhibits the formation of aPL IgG–β2GPI complexes. Still, the available data provide interesting clues regarding the mechanism of the effect. As indicated by dialysis experiments, the binding of HCQ to the protein(s) is weak and reversible. The drug appears to interact with both β2GPI and aPL IgG because it reversed the binding of the individual proteins to phospholipid and also reduced their affinities for the bilayer. The observations that a concentration of 1 mg/mL HCQ had an immediate effect whereas the concentration of HCQ at 1 μg/mL required preincubation with the proteins to see the effect suggest that the drug penetrates and binds to sites within the folded protein(s). It is also possible that HCQ may modify the tertiary structures of the proteins that are required for complexation. Slow protein unfolding events that occur over the course of minutes to hours have previously been described for other proteins.34
Although our experiments in which HCQ (1 mg/mL) was directly added to the bilayer and flushed away before the addition of the proteins showed no effect on the subsequent binding of complexes, the interpretation of these experiments is limited by the possibility that the HCQ did not remain bound to the lipid layer. Interestingly, it has been reported in an abstract that treatment of patients with elevated anticardiolipin antibody titers with hydroxychloroquine reduced the antibody titers,35 however other investigators did not observe a change in titer to correlate with use of the drug.36 The results of the current studies in which serum samples were spiked with 2 concentrations of HCQ—1 μg/mL and 1 mg/mL—indicates that the drug may decrease the apparent levels of these antibodies by reducing their binding to the cardiolipin-coated surfaces that are used for the assays. Modest, but statistically significant, effects were also noted for the β2GPI IgG and LA assays. The effect on the LA was evident only at the higher concentration of HCQ. The question of whether the effects of the drug on the clinical tests might relate to clinical efficacy in individual patients remains to be determined.
AFM has been previously used to study the effects of aPL antibodies and annexin A5 crystallization19 and to study the binding of β2GPI to phospholipid.29 To our knowledge, the present study is the first to use AFM imaging to observe the formation of aPL antibody–β2GPI complexes and to study the effects of HCQ on the structures. Interestingly, Gamsjaeger et al previously reported the formation of β2GPI structures, very similar to those described herein, and their binding studies using surface plasmon resonance suggested a 2-state reaction model, with fast binding of β2GPI to anionic phospholipid, followed by a slower phase of agglomeration on the bilayer surface.29 Our Kd determinations for the proteins, done at a physiologic calcium concentration, were within the ranges that they reported using surface plasmon resonance29 and that Willems et al reported using ellipsometry.17 In comparing the Kd for β2GPI to the previously reported values,29 it is important to note that the present studies, and also the AFM imaging, were performed using a physiologic calcium concentration of 1.25 mM and with phospholipid compositions of 30% phosphatidylserine and 70% phosphatidylcholine. It is attractive to speculate that the HCQ effect on β2GPI itself might be mediated by the binding of this amphiphilic drug to the lipid-binding region in complement control protein (CCP) domain V of the protein.37,38
HCQ has also been reported to reverse platelet activation induced by human IgG aPL antibodies,15 and to contribute to reduction of aPL antibody–induced thrombosis.14 Although the effect we describe may contribute to part of this process, the drug also has other platelet inhibitory properties.39 Among them, HCQ can inhibit collagen-induced platelet aggregation and alpha-granule release.40 The drug may also have a clinical antithrombotic effect in some postoperative clinical settings.41
The results of these experiments raise several additional questions that are the subjects of current and future research in our laboratory. A prime interest is the localization of the specific molecular targets of HCQ on the relevant proteins—β2GPI or aPL IgG—that may affect their forming complexes and binding to phospholipids. It will be important to know whether the HCQ-associated reduction of thrombosis that was observed in clinical studies and experimental models might be attributable to this effect of HCQ. It will be interesting to learn whether the reduction of binding of aPL antibodies to monocytes affects the activation that these antibodies have been reported to trigger.42,43 We previously showed that aPL antibodies disrupt annexin A5 crystallization,18,19,44 and it will be interesting to determine the effects of HCQ on this process. Finally, HCQ might also alter other antibody-antigen interactions, including autoantibody-antigen interactions involved in other autoimmune disease processes such as SLE and rheumatoid arthritis.
Current treatment of APS relies on anticoagulant drugs, which, as mentioned earlier, carry the risk of bleeding complications.5,45 These data clearly demonstrate that HCQ reverses the binding of IgG-β2GPI complexes to phospholipid bilayers. It may therefore be possible that HCQ, or other molecules with similar structures and chemical properties, may offer alternative approaches to treating APS that target a step in the disease mechanism that is earlier than the activation of coagulation reactions. Determination of the efficacy of HCQ treatment for APS would ultimately require formal prospective clinical trials.
In conclusion, we have provided clear evidence that HCQ can dissociate aPL IgG–β2GPI complexes from phospholipid bilayers. Additional studies will be needed to further define the molecular mechanism(s) for this dissociation and its possible role in modifying the APS disease process.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This study was supported by grant HL-61331 from the National Institutes of Health/the National Heart Lung and Blood Institute (Bethesda, MD).
National Institutes of Health
Authorship
Contribution: J.H.R. conceived the idea, designed the research, analyzed data, and edited the successive drafts of the paper; D.J.T. designed and directed the atomic force microscopy experiments, and wrote and edited the text; X.-X.W. prepared critical antibodies, designed and performed the ellipsometry, aCL IgG, and THP-1 cell line experiments, wrote an initial draft and prepared the manuscript for submission; A.S.Q. performed atomic force microscopy experiments and wrote relevant sections; P.P.C. prepared and characterized the monoclonal antibody, contributed to relevant methods and results sections, and edited the drafts; and J.J.H. contributed to the mathematic analysis of the protein interactions.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Jacob H. Rand, Core Laboratory Office, Foreman Pavilion 8, 111 East 210th Street, Bronx, NY 10467; e-mail: jrand@montefiore.org.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal