To the editor:
A recent report from the Center for International Blood and Marrow Transplant Research (CIBMTR) on the outcome of unrelated donor hematopoietic stem cell transplantation (HSCT) in first complete remission (CR1) of adult acute lymphoblastic leukemia (ALL) appropriately concluded that this treatment warranted further investigation.1 I would like to elaborate on some points that were discussed to a limited extent in the report.
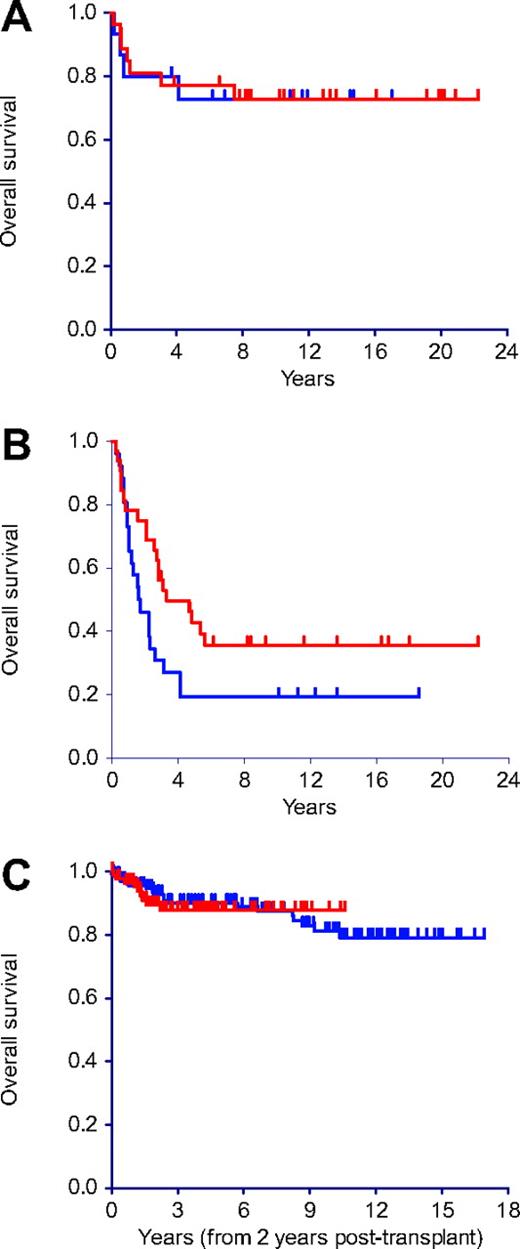
The contribution of a prolonged interval between achievement of CR1 and HSCT toward making outcomes seem better by excluding patients who relapse early cannot be overemphasized. This is especially relevant with unrelated donor transplantation where these intervals tend to be long; more than 3 months in two-thirds of the patients in the CIBMTR report. As Figure 1, derived from 100 adult ALL patients autografted in CR1,2 shows, this time-censoring effect may be particularly marked in patients with higher-risk disease who tend to relapse earlier (Figure 1). Because a substantial proportion of patients in the CIBMTR report had intermediate- or high-risk disease, it is conceivable that relatively long CR-transplantation intervals made a significant contribution to the magnitude of the favorable outcome.
Comparison of outcomes. (A) Lack of effect of the CR-transplantation interval on the outcome of ALL patients with low-risk disease (n = 42; 27 > 3 months, red; 15 ≤ 3 months, blue) autografted in CR1. (B) Beneficial effect of a longer CR-transplantation interval on the outcome of ALL patients with intermediate- or high-risk disease (n = 58; 32 > 3 months, red; 26 ≤ 3 months, blue) autografted in CR1 (P = .06). (C) Long-term survival of acute leukemia patients alive and well 2 years after allogeneic (blue) or autologous (red) transplantation in CR1 (P = .89).
Comparison of outcomes. (A) Lack of effect of the CR-transplantation interval on the outcome of ALL patients with low-risk disease (n = 42; 27 > 3 months, red; 15 ≤ 3 months, blue) autografted in CR1. (B) Beneficial effect of a longer CR-transplantation interval on the outcome of ALL patients with intermediate- or high-risk disease (n = 58; 32 > 3 months, red; 26 ≤ 3 months, blue) autografted in CR1 (P = .06). (C) Long-term survival of acute leukemia patients alive and well 2 years after allogeneic (blue) or autologous (red) transplantation in CR1 (P = .89).
When HSCT from HLA-identical siblings is evaluated,3 a donor versus no-donor comparison permits intention-to-treat analysis. However, this is not possible with unrelated donors. I propose applying a “correction factor” to compensate for the time-censoring effect.
In a recent major cooperative study of adult ALL,3 approximately 80% of patients were alive 6 months after enrollment. Because 6 months was also the median diagnosis-transplantation interval in the CIBMTR study, a crude way to apply a correction factor for the survival seen in this study may be to lower the survival estimate at any given time point by 20% of the projected figure. Thus, the 5-year survival of 39% could be considered to reflect an intent-to-treat 5-year survival probability of approximately 31.2% for an individual in whom an allograft is being considered. Similar correction factors should be applied to all reports of allogeneic HSCT from unrelated donors for the purposes of comparing treatment options, particularly for patients with acute leukemia.
The literature suggests that the efficacy of autotransplantation rivals that of unrelated or mismatched donor transplantation in a number of situations. Survival after autotransplantation in acute myeloid leukemia was found to be significantly higher than after unrelated donor transplantation among patients in CR1 and CR2.4 Survival after autotransplantation in CR1 ALL was found to be equivalent to unrelated donor transplantation, and marginally inferior in CR2.5 These data also originated from the CIBMTR. We have shown that the outcome of autotransplantation is superior to allogeneic transplantation from mismatched related donors for acute leukemia beyond CR1.6
Unlike with autografts, serious complications related to graft-versus-host disease may continue occurring for several years after allogeneic transplantation. We have shown that the 10-year survival probability of acute leukemia patients who are alive and well 2 years after an allograft is 81% compared with 89% for autograft recipients (Figure 1C).7,8
Unrelated donor transplantation consumes significant amounts of fiscal and nonfiscal resources, and results in considerable risk of morbidity and mortality with modest success rates. It also places altruistic individuals at some inconvenience and risk. It is therefore critical to use this intervention appropriately—in situations where no other realistic and simpler treatment is available.
Authorship
Conflict-of-interest disclosure: The author declares no competing financial interests.
Correspondence: Jayesh Mehta, MD, The Robert H. Lurie Comprehensive Cancer Center of Northwestern University, 676 N St Clair Street, Suite 850, Chicago, IL 60611; e-mail: j-mehta@northwestern.edu.