In this issue of Blood, Lu and colleagues describe a new method to differentiate human embryonic stem cells into large amounts of mature red blood cells.
Although the red blood cell supply is currently very safe, a donorless industrial process to manufacture red blood cells for transfusion is desirable. This would be beneficial because periodic shortages develop for rare blood groups and because the risk of contamination by new or emerging pathogens cannot be completely eliminated. Human embryonic stem cells (hESCs) or induced pluripotent stem cells can grow undifferentiated for long periods of time in vitro and are therefore a potentially unlimited source of cells from which red blood cells could be produced in large amounts if a method could be developed to efficiently induce hESC differentiation into adult red blood cells.
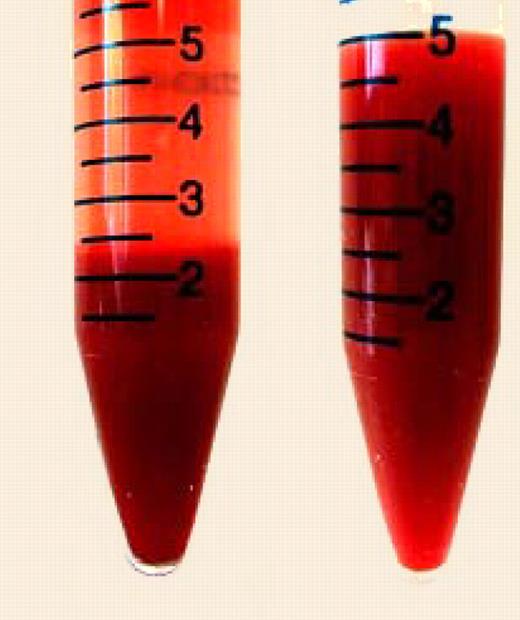
In vitro produced human embryonic stem cell-derived red blood cells. See the complete figure in the article beginning on page 4475.
In vitro produced human embryonic stem cell-derived red blood cells. See the complete figure in the article beginning on page 4475.
Lu and colleagues report in this issue of Blood that they have been able to produce large amounts of red blood cells from hESCs using a procedure that involves a combination of embryoid body formation in the presence of a cell-permeable recombinant HoxB4 transcription factor, amplification in liquid culture of hematopoietic and eryth-roid precursors, and final maturation and enucleation in the presence of feeder layer.
Several major issues must be resolved before the manufacture of red blood cells can become a reality. The first challenge that must be met is the development of a highly scalable and economically viable production method because the number of cells that is present in each unit of blood is considerable. Lu et al have produced over 10 billion cells, an unprecedented number for the field. In addition, several of the steps in their protocol should be scalable. This is an important achievement that provides a proof of principle that industrial production might one day be achievable. However, the number of cells necessary to cover even a small fraction of transfusion needs is several orders of magnitude higher than what has been achieved to date because a 220-mL unit of packed red blood cells contains about 2 trillion cells. Therefore, considerable biologic engineering remains to be done to reach the necessary scale at a reasonable cost. The final cost of red cell manufacturing will be highly dependent on the purity level and on the amount of testing that will be acceptable to the regulatory agencies.
A second challenge is to produce functionally normal cells. Three major types of red blood cells are produced during development that differ by morphology, size, and gene expression profiles, and by the type of hemoglobin produced. All current protocols to produce red cells from hESCs, including the one described by Lu et al, yield cells with an embryonic or fetal phenotype that are normally produced early in gestation.1 Whether such cells could be used for transfusion is unclear but seems unlikely, given the multiple differences that exist between adult and fetal or embryonic red cells. Coaxing hESCs into adult red cells therefore remains to be solved.
In addition to being at an appropriate developmental age, the cells obtained from hESCs should be fully functional. Lu et al show that the oxygen equilibrium curves of the hESC-derived cells are comparable to normal red blood cells and that the cells respond to changes in pH and 2,3-diphosphoglyerate. This is encouraging evidence that red blood cells produced from hESCs in vitro are relatively normal and in agreement with work done with hematopoietic stem cells.2 However, major questions, such as the half-life and the immunogenicity of these cells, must be addressed. Procedures to eliminate undifferentiated cells that could be tumorigenic must also be developed.
The first transfusions in modern times occurred more than 100 years ago, 70 years before the first transplantations because red blood cells are among the simplest cells present in the body. They are easy to harvest and store, do not express the HLA antigens, and do not have a nucleus. They are therefore less immunogenic than most cells and cannot cause tumors. Many of these same characteristics make them an attractive translational target for the hESC field. Importantly, most of the difficulties that are highlighted above apply to the manufacture of other cell types that have therapeutic potential. Therefore, the development of a procedure to manufacture red blood cells from hESCs would pave the way to the production of other cell types.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal