Abstract
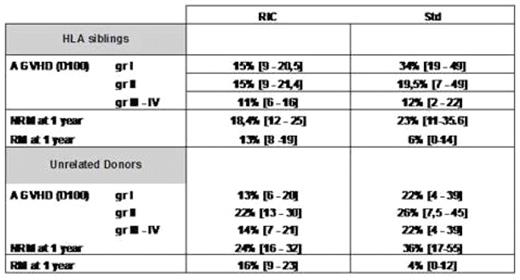
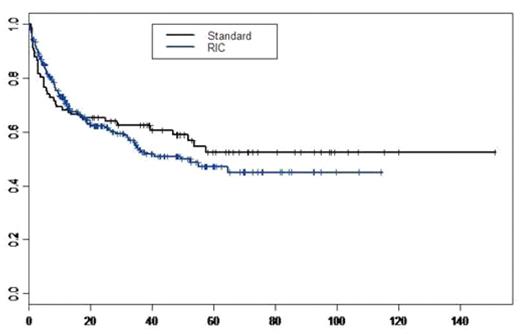
This retrospective analysis concerned 374 patients (pts) who underwent an allogeneic HSCT for CLL reported to the EBMT registry. There were 282 males (75%) and 92 females with a median age of 53 years (24–69). The interval between diagnosis and transplantation was 53 months (3–308). Forty-five pts (12%) have received a previous HSCT. At transplant, 302 among 323 evaluated patients had a good performance status (PS) (93%), 51 pts were in CR (14%), 163 in PR (45.5%), 39 in SD (11.5%) and 105 in PD (29%) among 353 evaluated patients. Two hundred and ninety-two pts received a standard (Std) and 82 a reduced intensity conditioning regimen (RIC); 314 pts received PBSC, 55 BM and 5 cord blood cells from 202 HLA siblings (Sib), 2 mismatched related donors and 170 unrelated donors (UD). There were 136 (36%) sex-mismatched (90 F/M and 46 M/F), 150 pairs (40%) had an ABO incompatibility (61 minor, 99 major) and for CMV: 80 pairs were +, 148− and 112 mixed. After transplantation, 359 pts engrafted, 201 pts developed an AGVHD (gr I: 76, gr II : 79, gr III: 30 and gr IV:16) and 153 presented a cGVHD (75 limited and 78 extensive). At day 100 after transplant, the cumulative incidence of AGVHD for the total population was 17% (13–22) for gr I, 31% (26–36) for gr ≥ II. [Sib: 19% (13–25) gr I and 27% (21–34) gr ≥ II; UD: 16% (9–22) gr I and 38% (29–47) gr ≥ II]. Results concerning the cumulative incidence of AGVHD according to HLA typing and kind of conditioning are shown in Table I. At 1 year after transplant for the total population, the cumulative incidence of limited and extensive cGVHD were 15 % (6–24) and 29.5% (18–41) for Std; 18.6 (13–24) and 18% (13–23) for RIC respectively. With a median follow up of 38 months, the probability of 3-year and 5-year overall survival (OS) and disease-free survival (DFS) for the total group were 56% (51–62) and 47.4 % (42–53); 49 % (43–56) and 42% (36–48.5) respectively. We observed a significant difference concerning 5-year OS according to the pretransplant disease status [CR: 73% (60–89), PR: 57% (48–68) and PD: 35% (26–46)] (p<0.00001). There was no significant difference between standard and RIC HSCT in term of OS with 52.4 % (42–66) and 47% (40–55.5) respectively (p=0.44) (Figure 1) [Std and RIC Sib: 51% (37–70) and 56% (47–67); Std and RIC UD: 60% (44–83) and 40% (29–55) respectively]. The multivariate analysis using Cox model showed a significant impact of 3 factors on OS: age: HR=1.061 (1.02–1.10) p<0.0001, gender: HR=2.29 (1.02–5.11) p=0.04 and PS: HR=3.15 (1.40–7.10) p=0.005. The cumulative incidence of non-relapse and relapse mortality (NRM and RM) at 3 months and 1 year after transplant were: 10 % (7–13), 5% (3–7) and 24% (19–28), 15% (12–19) respectively [Std:23 % (11–35.6), 6% (0–14) 1 year; RIC: 22.5% (17.5–27), 18% (13–22) at 1 year]. Results concerning the cumulative incidence of NRM and RM according to HLA typing and kind of conditioning are shown in Table I. This large retrospective analysis showed a high percentage of long-term OS after HSCT for CLL either after Std or RIC conditioning without any difference between the 2 groups except for the AGVHD (gr I, III and IV) where we had an higher incidence in the Std group, and for the RM with a higher level in the RIC group. Moreover, we demonstrated the important impact of disease status pretransplant (univariate); age, PS and sex-matching (multivariate) on the global OS.
Table 1: cumulative incidence of AGVHD, NRM and RM according to HLA typing and kind of conditioning
Probability of OS for Standard conditioning group and RIC group
Probability of OS for Standard conditioning group and RIC group
Disclosures: No relevant conflicts of interest to declare
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal