Abstract
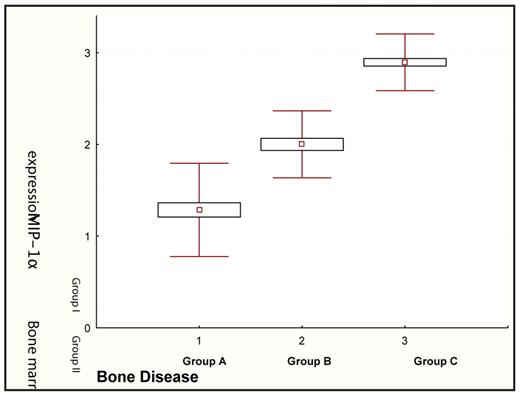
Macrophage inflammatory protein-1 alpha (MIP-1alpha) is a low molecular weight chemokine that belongs to the RANTES family and is a potent osteoclast stimulator. Previous studies have shown that malignant plasma cells (PCs) from myeloma cell lines produce MIP-1alpha, while MIP-1alpha levels are elevated in the bone marrow plasma and the serum of patients with multiple myeloma (MM) and correlate with the extent of bone disease. The purpose of our study was to evaluate the role of MIP-1alpha immunoexpression on bone marrow trephine biopsies in myeloma bone disease and examine possible correlations between MIP-1alpha expression with survival and prognostic factors of MM. We evaluated formalin fixed paraffin-embedded bone marrow sections of 130 patients with newly diagnosed MM (66M/64F, median age: 68 years). Bone marrow sections were subjected to immunohistochemistry study using the anti-MIP- 1alpha monoclonal antibody (Santa Cruz Biotechnology Inc., Santa Cruz, CA, USA). The immunoreactivity of MIP-1alpha was examined on the basis of positive PCs with the following cut off values: <20% positive PCs (negative expression group, group I), 20–50% positive PCs (intermediate expression group, group II) and >50% positive PCs (high expression group, group III). Moreover MIP-1alpha was measured using ELISA methodology (R&D Systems, Minneapolis, MN, USA) in the serum of the patients. The extent of bone disease was assessed radiographically, and grading was performed as follows: group A included 43 patients (33%) who had no lytic lesions and/or osteoporosis only, group B included 24 patients (18%) who had lytic lesions in 1–3 areas, whereas group C included 63 patients (48%) with lytic lesions in >3 areas and/or a bone fracture. Thirty-seven (28%) patients had negative MIP-1alpha expression, 17 (13%) intermediate expression and 79 (59%) high expression of MIP-1alpha. MIP-1alpha expression of ≥20% PCs in the trephine biopsies significantly correlated with the extent of bone disease (Figure 1, ANOVA p<0.0001). Furthermore, 91 patients (70%) had values of serum MIP-1alpha >14 pg/ml, which was the median value observed in 20 controls of similar age and gender (p<0.001). MIP-1alpha serum levels also correlated with the extent of bone disease (ANOVA p<0.0001). In terms of overall survival, no significant association was observed in relation to MIP-1alpha expression. Increased immunoexpression of MIP-1alpha was associated with high plasma cell infiltration in the bone marrow (r=0.348, p<0.0001), low platelet count (r=0.282; p=0.0012), hypercalcemia (r=0.246; p=0.022), elevated serum creatinine (r=0.258, p=0.027), and advanced disease stage (ISS, p=0.034). Our findings underline, for the first time, the increased incidence of high immunoexpression of MIP-1alpha in the malignant PCs of myeloma patients and the correlation between the expression of MIP-1alpha by myeloma PCs in the trephine biopsies and the extent of lytic bone disease. These results confirm the significant role of MIP-1alpha in the pathogenesis of myeloma bone disease and suggest that MIP-1alpha may represent a rational therapeutic target for the management of bone destruction in myeloma.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal