Abstract
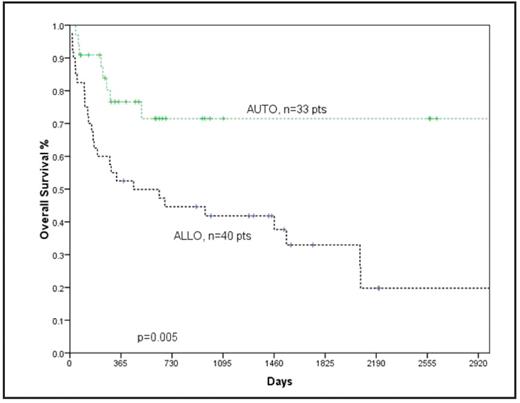
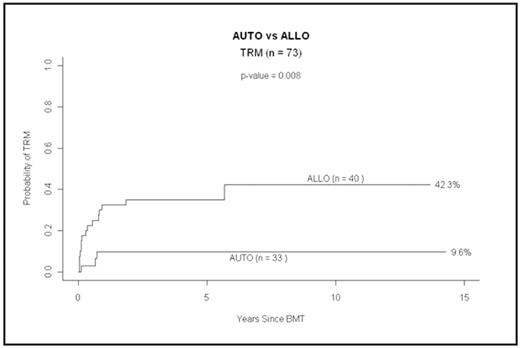
There is no literature comparing the outcome of autologous vs allogeneic SCT as a salvage therapy for refractory/relapsed transformed lymphoma. We therefore evaluated 73 patients with refractory/relapsed transformed and composite lymphoma (TNHL) treated with either autologous (AUTO) (n=33, 45%) or myeloablative allogeneic (ALLO) (n=40, 55%) SCT between Jan 89 and Oct 07 in this single center, population based study. We hypothesized that patients would fare better with allo SCT due to lower relapse risk. The median follow up for surviving patients treated with AUTO SCT is 21 m (range: 3–174 m) and with ALLO 48 m (rang: 12–166 m). Baseline characteristics for the 2 groups are outlined in the table. The ALLO group had a significantly higher proportion of patients with advanced stage NHL and IPI of 2 or more at the initial diagnosis. The 2- and 5-y OS for the whole group is 55% and 46% respectively. The 1-y cumulative incidence (CI) of relapse and therapy related mortality (TRM) for the whole group is 30% and 26% respectively. Twenty-six of 33 patients (79%) treated with AUTO and 13 of 40 pts (33%) treated with ALLO are alive. OS for the AUTO and ALLO groups at 2-y is 72% vs 45% and at 5-y 72% vs 33% respectively, (p=0.005). EFS for the AUTO and ALLO groups at 2-y is 47% vs 38% and at 5-y 33% vs 29% respectively, (p=0.39). The risk of disease relapse at 5 yr is non-significantly lower in the ALLO compared to the AUTO group at 36 vs 57% (p=0.1). CI of disease relapse for the AUTO and ALLO groups at 1-y is 31% vs 23% and at 5-y 57% vs 36% respectively, (p=0.1). TRM was however significantly lower for the AUTO compared to the ALLO group with 1- and 5-year CI - TRM at 10% vs 33% and 10% vs 35% respectively, (p=0.008). Evaluation of these 2 cohorts suggest that the higher TRM of allografting in this group of lymphoma patients is not overcome by a compensatory improvement in relapse risk. Use of myeloablative ALLO SCT did not result in superior OS when compared to use of AUTO SCT for patients with refractory/relapsed transformed lymphoma. Moreover, we did not observe a plateau in the survival curve with use of ALLO SCT. Whether this situation may be improved with use of AUTO followed by non-myeloablative or reduced intensity ALLO SCT remains to be determined.
Table 1: Baseline characteristics of the autologous and allogeneic groups.
| Parameter . | AUTO group (%) . | ALLO group (%) . | p value . |
|---|---|---|---|
| *at diagnosis | |||
| Patient number | 33 (45) | 40 (55) | |
| Gender: Male/Female; Ratio | 22/11; 2:1 | 27/13; 2:1 | 0.88 |
| Age (years): Median/Range | 53/25–70 y | 44/30–85 y | 0.34 |
| Prior rituximab therapy | 19 (58) | 14 (35) | 0.12 |
| Stage: * | |||
| limited/advanced | 5/22 (15/67) | 3/36 (8/90) | 0.009 |
| IPI (number of factors)* | 0.03 | ||
| 0/1 | 16 (48) | 18 (45) | |
| 2/3 | 7 (21) | 18 (45) | |
| 4/5 | 0 (0) | 2 (5) | |
| Parameter . | AUTO group (%) . | ALLO group (%) . | p value . |
|---|---|---|---|
| *at diagnosis | |||
| Patient number | 33 (45) | 40 (55) | |
| Gender: Male/Female; Ratio | 22/11; 2:1 | 27/13; 2:1 | 0.88 |
| Age (years): Median/Range | 53/25–70 y | 44/30–85 y | 0.34 |
| Prior rituximab therapy | 19 (58) | 14 (35) | 0.12 |
| Stage: * | |||
| limited/advanced | 5/22 (15/67) | 3/36 (8/90) | 0.009 |
| IPI (number of factors)* | 0.03 | ||
| 0/1 | 16 (48) | 18 (45) | |
| 2/3 | 7 (21) | 18 (45) | |
| 4/5 | 0 (0) | 2 (5) | |
OS for patients with transformed NHL post autologous and myeloablative allogeneic SCT
OS for patients with transformed NHL post autologous and myeloablative allogeneic SCT
CI of TRM for patients with transformed NHL post autologous and myeloablative allogeneic SCT
CI of TRM for patients with transformed NHL post autologous and myeloablative allogeneic SCT
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal