Abstract
130 patients who were unsuitable for conventional-intensity conditioning underwent RI-HSCT after 100 mg/m2 melphalan (+ 50 mg/kg cyclophosphamide if no prior autograft). GVHD prophylaxis comprised cyclosporine (HLA-matched siblings) or tacrolimus (all others) and MMF.
Table 1: Patient characteristics
| Age (y) . | 19–71 (median 55) . |
|---|---|
| Male | 55% |
| Refractory disease | 57% |
| ECOG performance status | 0 34% |
| 1 48% | |
| 2 14% | |
| 3 4% | |
| Diagnosis | Lymphoma 42% |
| Leukemia 36% | |
| Myeloma 22% | |
| Donor | Matched sibling 49% |
| Mismatched sibling 2% | |
| Matched unrelated 33% | |
| Mismatched unrelated 15% | |
| Donor age (y) | 21–71 (median 44; 45% >45) |
| Male donor | 65% |
| Prior autograft | 45% |
| Age (y) . | 19–71 (median 55) . |
|---|---|
| Male | 55% |
| Refractory disease | 57% |
| ECOG performance status | 0 34% |
| 1 48% | |
| 2 14% | |
| 3 4% | |
| Diagnosis | Lymphoma 42% |
| Leukemia 36% | |
| Myeloma 22% | |
| Donor | Matched sibling 49% |
| Mismatched sibling 2% | |
| Matched unrelated 33% | |
| Mismatched unrelated 15% | |
| Donor age (y) | 21–71 (median 44; 45% >45) |
| Male donor | 65% |
| Prior autograft | 45% |
Refractory disease, HLA mismatch, donor age >45, elevated creatinine, low DLCO, thrombocytopenia, male donor, poor performance status, and low albumin affected OS adversely in univariate analysis. The following factors affected outcome independently:
Table 2: Cox analysis
| Adverse variable . | Relative risk . | P . |
|---|---|---|
| TRM | ||
| HLA mismatch | 4.78 | 0.0003 |
| Performance status 2–3 | 3.07 | 0.044 |
| Relapse | ||
| Donor age >45 y | 2.0 | 0.012 |
| Male donor | 1.98 | 0.026 |
| Refractory disease | 1.84 | 0.05 |
| EFS | ||
| Performance status 2–3 | 0.48 | 0.022 |
| HLA mismatch | 0.53 | 0.023 |
| Refractory disease | 0.55 | 0.016 |
| Male donor | 0.61 | 0.039 |
| Donor age >45 y | 0.63 | 0.034 |
| OS | ||
| Performance status 2–3 | 0.44 | 0.025 |
| HLA mismatch | 0.31 | 0.0001 |
| Refractory disease | 0.49 | 0.007 |
| Donor age >45 y | 0.55 | 0.012 |
| High LDH | 0.53 | 0.007 |
| Platelets <100 | 0.58 | 0.021 |
| Adverse variable . | Relative risk . | P . |
|---|---|---|
| TRM | ||
| HLA mismatch | 4.78 | 0.0003 |
| Performance status 2–3 | 3.07 | 0.044 |
| Relapse | ||
| Donor age >45 y | 2.0 | 0.012 |
| Male donor | 1.98 | 0.026 |
| Refractory disease | 1.84 | 0.05 |
| EFS | ||
| Performance status 2–3 | 0.48 | 0.022 |
| HLA mismatch | 0.53 | 0.023 |
| Refractory disease | 0.55 | 0.016 |
| Male donor | 0.61 | 0.039 |
| Donor age >45 y | 0.63 | 0.034 |
| OS | ||
| Performance status 2–3 | 0.44 | 0.025 |
| HLA mismatch | 0.31 | 0.0001 |
| Refractory disease | 0.49 | 0.007 |
| Donor age >45 y | 0.55 | 0.012 |
| High LDH | 0.53 | 0.007 |
| Platelets <100 | 0.58 | 0.021 |
These prognostic factors were similar to those found on studying the first 63 patients in this series (Mehta et al. Bone Marrow Transplant 2006) –with the additional emergence of HLA mismatch and thrombocytopenia which were significant in univariate but not multivariate analysis then.
These data suggest that RI-HSCT is useful for some patients with hematologic malignancies who are ineligible for conventional-intensity HSCT. However, alternative HSCT techniques or non-HSCT options are needed for high-risk patients.
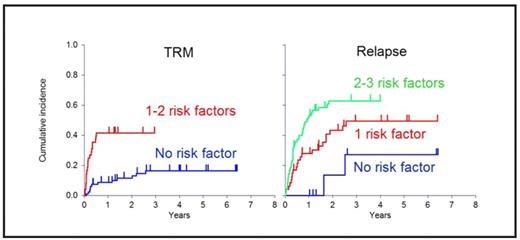
shows the effect of the number of adverse prognostic factors on the cumulative incidence of relapse and transplant-related mortality.
shows the effect of the number of adverse prognostic factors on the cumulative incidence of relapse and transplant-related mortality.
shows the effect of the number of adverse prognostic factors on survival.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author


This feature is available to Subscribers Only
Sign In or Create an Account Close Modal