Abstract
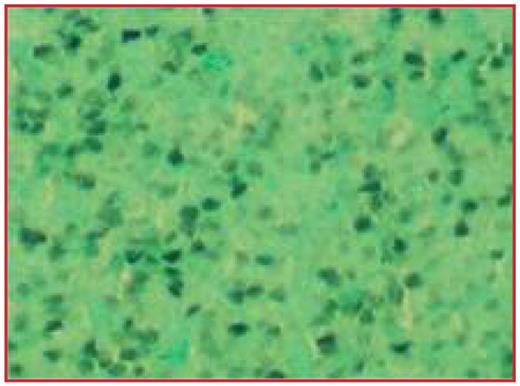
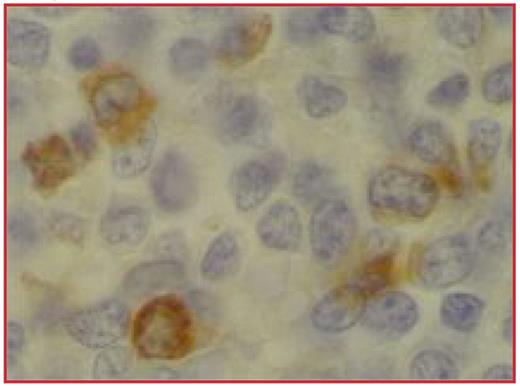
Acute biphenotypic leukemia (ABL) represents a minority of acute leukemia cases (around 5%) in which blasts co-express markers of different lineages (myeloid, T-cell or B-cell). ABL without bone marrow involvement is exceedingly rare. Case report: An 18-year-old man presented with slowly enlarging, non-tender cervical lymph nodes. He had no other symptoms. Family history included Hodgkin’s disease in his mother and maternal great aunt, histiocytosis X in his maternal cousin, and non-Hodgkin’s lymphoma in his paternal grandfather. Physical exam revealed multiple small cervical and axillary lymph nodes. Laboratory analyses including complete blood count, peripheral blood smear, complete metabolic profile, mononucleosis screen, and hepatitis and HIV serologies were unremarkable. Histopathological examination of the left cervical lymph node revealed rare germinal centers with an interfollicular proliferation of generally medium size cells with a fine blastic chromatin pattern and scant cytoplasm. CD34 was positive in more than half of the cells. Between 30% and 80% of the cells were positive for TdT (Figure 1), CD3, CD4, and CD7. Myeloperoxidase (Figure 2) and lysozyme were positive in about 20% of the cells. Flow cytometry revealed an immature myeloid cell population coexpressing CD33, CD13, CD7, and CD34. Chromosomal analysis revealed a complex karyotype. Bone marrow exam was unremarkable and no evidence of leukemia was observed. Flow cytometry of the bone marrow aspirate revealed only 4% of the cells to be CD34+. Whole body PET scan showed extensive uptake in bilateral axillae, neck, and inguinal regions without any extranodal involvement. The patient received hyper-CVAD regimen (alternating cycles of cyclophosphamide, vincristine, adriamycin, dexamethasone and high dose methotrexate, cytarabine) for 8 cycles and remains in remission five months after the end of hyper-CVAD protocol. To our knowledge, this is the third case reported in the literature with acute biphenotypic leukemia not involving the bone marrow. However, our case cannot accurately be referred to as leukemia since the bone marrow is not involved; neither can it be named as lymphoblastic lymphoma because of its myeloid differentiation. Therefore, we will refer to it as extramedullary granulocytic sarcoma with biphenotypic features.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal