Abstract
Despite dramatic gains in life expectancy in the desferrioxamine era for thalassemia major patients, the leading cause of death for this young adult’s population remains iron-induced heart failure. For this reason, strategies to reduce heart disease by improving chelation regimens have the highest priority in this phase. These strategies include development of novel oral iron chelators to improve compliance. Oral deferipron was proved more effective than subcutaneous desferrioxamine in removing cardiac iron. The novel oral one-daily chelator deferasirox has been recently commercially available but its long-term efficacy on myocardial iron concentrations and cardiac function is unknown. Aim of this study was to compare in thalassemia major patients the effectiveness of deferasirox, deferipron, and desferrioxamine on myocardial and liver iron concentrations and bi-ventricular function by quantitative magnetic-resonance imaging (MRI).
Among the 550 thalassemic subjects enrolled in the MIOT (Myocardial Iron Overload in Thalassemia) network between September 2006 and September 2007, we selected patients receiving one chelator alone for longer than one year. MIOT is an Italian network of six MR sites where the cardiac and liver iron status is assessed by validated and homogeneous standard procedures. We identified three groups of patients: 24 treated with deferasirox, 42 treated with deferipron and 89 treated with desferrioxamine. The three groups were matched for gender, Hb pre-transfusion levels, age of starting chelation, and good compliance to the treatment. The deferasirox group was significantly younger (26±7 years) than the deferipron (32±9 years) and desferioxamine group (33±8 years) (P=0.0001) and showed significantly higher mean serum ferritin levels (2516±2106 ng/ml) than the deferipron (1493±1651 ng/ml) and the desferrioxamine group (987±915 ng/ml) (P=0.0001). Myocardial iron concentrations and distribution were measured by MRI T2* multislice multiecho technique. Biventricular function parameters were quantitatively evaluated by cine-dynamic MRI images. Liver iron concentrations were measured by MR T2* multiecho technique. Written informed consent was obtained from all subjects.
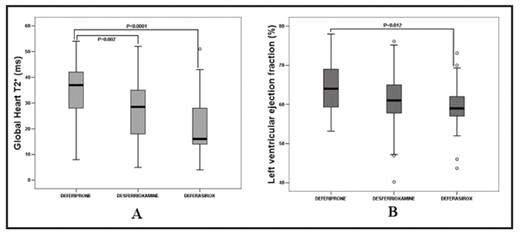
The global heart T2* value was significantly higher in the deferipron group (34±11 ms) versus the deferasirox (21±12 ms) and the desferrioxamine group (27±11 ms) (P=0.0001), as showed in Figure A. The T2* in the mid ventricular septum was significantly higher in the deferipron (36 ± 12 ms) versus the deferasirox (20 ± 12 ms) and the desferrioxamine group (28 ± 13 ms) (P = 0.0001). The number of segments with normal T2* value was significantly higher in the deferipron and the desferrioxamine group versus the deferasirox group (14 ± 2 versus 11 ± 6 versus 7 ± 7 segments; P = 0.0001). Among the biventricular function parameters, we found higher left ventricular ejection fractions in the deferipron and the desferrioxamine group versus the deferasirox group (64 ± 7 versus 62 ± 6 versus 58 ± 7 %; P = 0.005), as showed in Figure B. Liver T2* values were significantly higher in the desferrioxamine group versus the deferipron and the deferasirox group (10 ± 9 versus 6 ± 6 versus 5 ± 5 segments; P = 0.002).
In conclusion, Oral deferipron seems to be more effective than oral deferasirox and subcutaneous desferrioxamine in removal of myocardial iron with concordant positive effect on left global systolic function.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal