Abstract
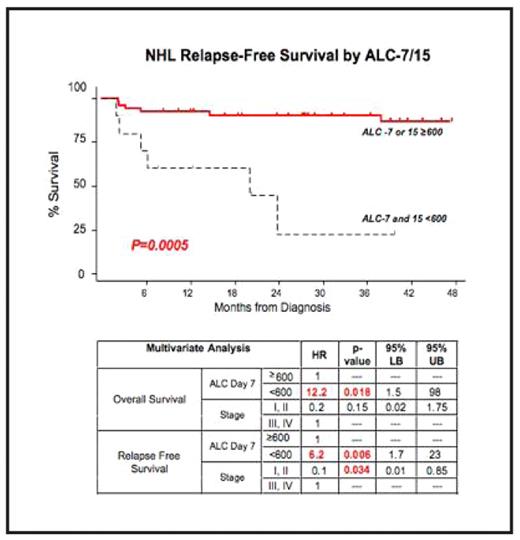
A role for the immune system during treatment for cancer therapy has not been widely established. However, we have previously reported that lymphocyte counts during chemotherapy independently predict outcome in pediatric patients with acute lymphoblastic leukemia (ALL), acute myelogenous leukemia, and Ewing’s sarcoma. Others have reported similar observations in adults with AML, follicular lymphoma and diffuse large B cell lymphoma. This led us to evaluate the prognostic ability of lymphocyte counts in pediatric patients with non-Hodgkin’s lymphoma (NHL). Seventy-six consecutive patients with de novo NHL, age 1–21 years, who were treated at M. D. Anderson Cancer Center were reviewed. We analyzed absolute lymphocyte counts (ALC) at diagnosis and days 7, 15, 21 and 28 of induction chemotherapy. We found that similar to children with ALL, lymphocyte counts in young patients with NHL during induction chemotherapy are independently prognostic for both overall survival and relapse-free survival. For example, children with low ALC on day 7 (ALC-7) of induction had poor RFS and OS. Specifically, patients with ALC-7 <600 cells/μL had a 2-year RFS of 56% versus 95% for those with ALC-7 >600 cells/mcL (HR=4.4, p=0.003). Strikingly, the 19% (12/63) of children with low ALC on both day 7 and 15 (<600 cells/mcL) had a 2-year RFS of 23% compared with 90% for those with either an ALC-7 or -15 >600/mcL (HR=8, p=0.0004). This effect was so dramatic that when ALC-7 of treatment was evaluated as a continuous variable, each cell/mcL increase in ALC was protective for OS decreasing the hazard ratio by 0.002 (p=0.04–0.05). This predicts that an increased ALC of only 250 cells/mcL would yield an HR of 0.5. Importantly, in multivariate analysis with disease stage (I+II versus III+IV), ALC-7<600 remained significantly prognostic for OS and RFS (HRs 6.2–12.2, p=0.006–0.018). Interestingly, lymphocyte counts prior to starting treatment also were prognostic with ALC<500–1000/mcL predicting poor OS (HRs 3.4–4, p=0.04–0.05).
These data reveal that low lymphocyte counts prior to and during induction chemotherapy in children with NHL are significant independent predictors of poor prognosis. These findings support a potential role for the immune system in the treatment of pediatric NHL which should be explored. Outcome differences of 39% are highly clinically relevant and suggest that ALC during induction should be evaluated prospectively and may contribute to future risk stratification of pediatric NHL.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal