Abstract
Background: In patients with aggressive NHL, whole-body positron emission tomography/computed tomography (PET/CT) with [18F]fluorodeoxyglucose (FDG) performed after 2–4 cycles of front-line therapy has a reported positive predictive value (PPV) of 80–100% and a negative predictive value (NPV) of 70–100%. However, the studies reporting these results were primarily retrospective, contained a mixture of NHL subtypes and therapies, and did not apply the recently published consensus response criteria (
Methods: In this study, patients with a new diagnosis of advanced stage diffuse large B-cell lymphoma (DLCL) received standard R-CHOP × 6 cycles. Patients had FDG-PET/CT scans performed after cycle 2 or 3 and at the completion of therapy. Two medical oncologists (AC, NB) reviewed the FDG-PET/CT reports and interpreted them as positive, negative, or equivocal. A nuclear medicine radiologist (FD) then reviewed the scans and applied the consensus response criteria to score each FDG-PET/CT as positive or negative. All patients provided written informed consent.
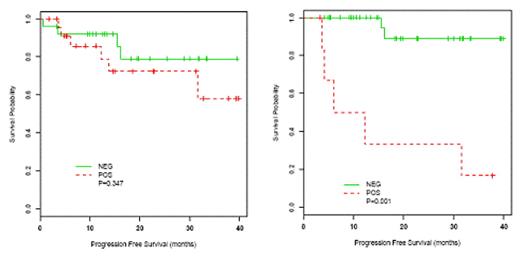
Results: Fifty patients (mean age 58 years, range 29–80) with stage III (n=15) or IV (n=35) DLCL were enrolled between March 2005 and May 2008 and treated with R-CHOP. All patients had a FDG-PET/CT performed after cycle 2 (n=47) or 3 (n=3), and 42 patients had FDG-PET/CT after 6 cycles. Median follow-up is 15 months. The medical oncologists interpreted the post-cycle 2 FDG-PET/CT reports as follows: 15 (30%) positive, 15 (30%) negative, 20 (40%) equivocal. Their NPV was 87% and the PPV was 27%. Patients with equivocal scans had outcomes similar to those with negative scans (80% free of relapse). After the radiologist’s review, the equivocal scans were classified as negative (n=10, 50%) or positive (n=10, 50%). The reviewed post-cycle 2 PET/CT results did not significantly correlate with progression-free survival (PFS) (graph, log-rank test p-value=0.35), and NPV and PPV were 85% and 25%, respectively. At the completion of therapy, the medical oncologists called 5 (12%) FDG-PET/CT reports positive, 25 (60%) negative, and 12 (29%) equivocal. These results significantly correlated with PFS (logrank test p-value<0.001; NPV 92% and PPV 80%). Again, the equivocal scans predicted outcomes similar to negative scans (92% free of relapse). The final, radiologist-reviewed FDG-PET/CT results were also significantly associated with outcome (graph, log-rank test p-value<0.001).
Conclusions: In contrast to prior reports on the value of interim FDG-PET/CT, our results demonstrate that in DLCL patients treated with R-CHOP who are assessed prospectively, interim FDG-PET/CT does not predict PFS. However, end of therapy FDG-PET/CT does correlate strongly with PFS. It may be that the dichotomous consensus response criteria, which apply to end of therapy FDG-PET/CT, are not useful for interpretation of interim scans. In support of a more relative interpretation of interim FDG-PET/CT, we found that the subset of FDG-PET/CT reports that cannot be clearly designated as positive or negative predict outcomes similar to those of negative scans.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal