Abstract
Background: Against the background of patient involvement, understanding patients’ preferences for treatments is crucial: Do physicians have the same or a different perception of the patients’ preferences? In the present study, physicians’ beliefs about patients’ preferences regarding the treatment of multiple myeloma (MM) were explored in a direct assessment, a Discrete-Choice-Experiment (DCE) and compared to the patients’ views.
Patients and methods: In a preceding study with MM-patients, relevant attributes of an ideal MM-treatment were collected by reviewing the literature and by conducting a qualitative study with focus groups. The attributes were analyzed in a subsequent quantitative study with self-completed paper-pencil or online questionnaires using both a direct measurement (16 items on a five-point Likert-scale) and a DCE (eight pairs with eight characteristics). In the present study, 243 physicians answered (76% male, 62% haematology specialists, 70% with >10 MM-patients in the last 12 months) the identical questionnaire except for the supplementary attribute “non-impaired sexuality” in the direct measurement.
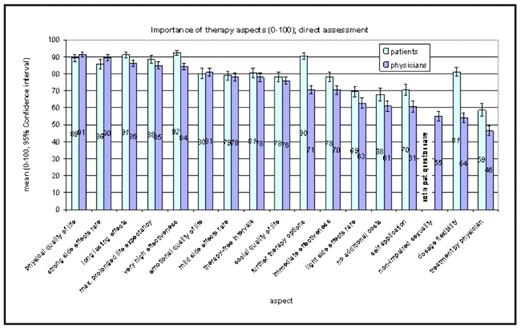
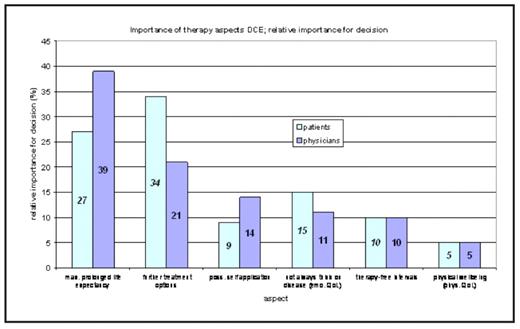
Results: Figure 1 shows the results of the direct measurement of preferences including confidence intervals. Physicians rated physical quality of life (specified as “reduced mobility or good mobility”), rare side effects and effectiveness aspects (duration of effect, maximal prolonged life expectancy and effectiveness) as most important attributes from the patients’ perpective, followed by emotional quality of life (specified as “Not always think of the disease”) and therapy-free-intervals. Especially further treatment options and dosage were more important to patients than physicians think. While the direct assessment gathers a range of important aspects, weighing particular relevant treatment attributes in a DCE is important. Physicians ranked prolonged life expectancy as most relative important and significantly more important than all other treatment attributes (as shown in figure 2). Further treatment options were second most important and significant compared to breaks in therapy and physical quality of life, whereas the patients ordered these two top priorities reversely. Similarly, the patients gave the opposite relative importance to the next two priorities: self-application of treatment and emotional quality of life.
Conclusion: Whether asking patients or physicians about the MM-patients’ treatment preferences, the combination of direct assessment and DCE proves as a valid survey technique. Over a broad range of treatment attributes the physicians’ perceptions of preferences were very close to those of MM patients. However in the DCE, after weighing the attributes patients assigned a higher relative importance to further treatment options and “Not always think of the disease”, but less to prolonged life expectancy and self-application.
Disclosures: Ortho-Biotech, Division of Janssen-Cilag GmbH Germany supported this research. Disclosures: Muehlbacher:Janssen Cilag GmbH: Research Funding. Berndt:Janssen-Cilag GmbH: Employment. Schreder:Janssen-Cilag GmbH: Employment. Nuebling:Janssen Cilag GmbH: Research Funding.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal