Abstract
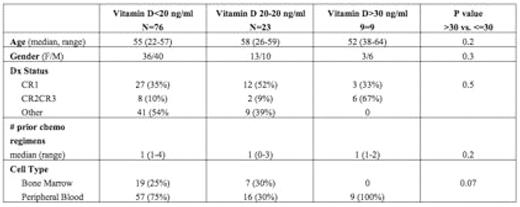
Vitamin D deficiency has long been understood to place patients at increased risk for reduced bone density and the development of pathological fractures. In addition to these classical manifestations, a wide body of emerging evidence suggests that Vitamin D deficiency may also increase the risk of illnesses associated with inflammation, including cardiovascular disease, infectious disease, autoimmune disease, and many common cancers. Our own in vitro data has confirmed that Vitamin D receptors are sharply upregulated on activated T cells and that physiologic calcitriol concentrations appear to have direct immunomodulatory functions (Joseph and Komanduri, unpublished). Vitamin D sufficiency is estimated by measuring 25-hydroxyvitamin D (25-OH D or calcidiol), and although there is no consensus on the optimal levels, many clinicians define sufficiency as >30 ng/ml, insufficiency as 20–30 ng/ml, and deficiency as <20 ng/ml. As one of the main sources of Vitamin D is through exposure to sunlight, allogeneic stem cell transplant (SCT) patients are at especially high risk of developing Vitamin D deficiency secondary to prolonged hospitalizations and standard recommendations to avoid sun exposure due to their increased risk of photosensitivity. To our knowledge, there are no large studies describing the incidence of Vitamin D deficiency in allogeneic SCT patients. We initially conducted a pilot study to assess Vitamin D levels in a group of allogeneic SCT recipients approximately assessed at approximately post-SCT day +100 (n=71) and found that only 18% of patients were sufficient, while the incidence of deficiency and insufficiency were to be 62%, and 20% respectively. To further elucidate if the deficiency was present pre-transplant or occurred post-transplant because of hospitalization and avoidance of sun exposure, we then assessed pre-transplant 25-hydroxyvitamin D levels in a larger group of allogeneic SCT recipients (n=108), and found that only 8% had normal baseline levels, while the vast majority were deficient (71%) or demonstrated insufficiency (21%). The baseline characteristics of this population are shown in the table below. Although this pilot study was not designed to assess the clinical significance of Vitamin D deficiency in the allogeneic transplant population, we believe that the unexpectedly high incidence of Vitamin D deficiency in SCT recipients deserves further study. Given the increasing epidemiologic and laboratory data implicating the Vitamin D axis in inflammation, we plan to assess traditional clinical outcomes associated with deficiency (including bone density and fracture rates) as well as immunological endpoints (GVHD and infection incidence) in future longitudinal studies. In conclusion, the incidence of Vitamin D deficiency in the allogeneic transplant setting is very high and additional studies are warranted to determine the clinical consequences associated with deficiency, and the potential therapeutic benefits of Vitamin D repletion in SCT recipients.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal