Abstract
Background; although numerous studies have described ID in the short-term post transplant, few include data on long-term ID following allo-SCT.
Aim; describe longitudinally the evolution of T-, B-, and NK-cells in a cohort of 140 consecutive pts following allo-SCT and to correlate this evolution with the advent of late clinical infections.
Patients & Methods; 140 pts with a median follow-up of 38 months (mo) were studied [median age 27 (39 less than 16) & 77% with malignancies]. Bone marrow (81%) from sibling (66%) was used before MA conditioning regimen (TBI 42%). 51% had grade II–IV acute- and 30% extensive-GvHD. All pts were monitored before and at 3, 6, 12, & 24 mo post transplant for both CD4 & CD8 subsets [CD45RA (naïve), 45RA+62L- (terminally differentiated), 45RO+ (memory), 28+ (competent), and Dr+ (activated)],NK cells (CD3-, 16+56+), and B cells CD19+/5+, 19+/27- (naives) and 19+27+ (memory).
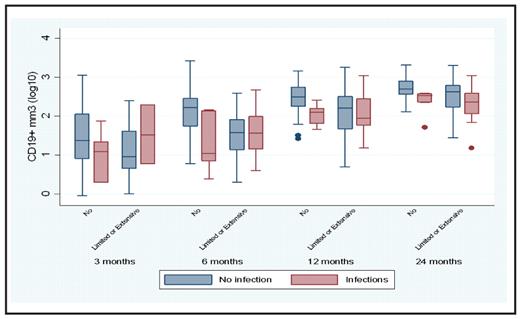
Results; we observed; for both CD4 CD8 a 1- year ID of the naive, memory and competent and above limits value for competent subsets; NK normalization at 6 mo; expansion of CD19+/5+ after 3 mo and persisting (till 24 mo) ID of memory B cells. Chronic GvHD did not influence significantly those parameters for CD8 subsets while strongly affecting the naïve and competent CD4 subsets, but the most profound defect was on B cell subsets especially on memory B. Contrasting this profound ID the cumulative incidence of late severe infections (LSE) was rather low (14% at 4 years). The only clinical factor that was marginally statistically linked to these was the use of PBSC instead of marrow. We then finally constructed Cox models to search for putative clinical or immunological risk factors for these LSE. Only low B cell counts at 6 (p=.05) & 24 mo (p=.016) were associated with the hazard of developing SLE, in particular if patients did not developed chronic GvHD (see Figure)
Conclusion; despite a long lasting ID post transplant following MA conditioning the rate of LSI remains low with modern antimicrobial prophylaxis; only B cell defect correlated with LSI despite immunoglobulin supplementation in pts with low Ig level.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal