Abstract
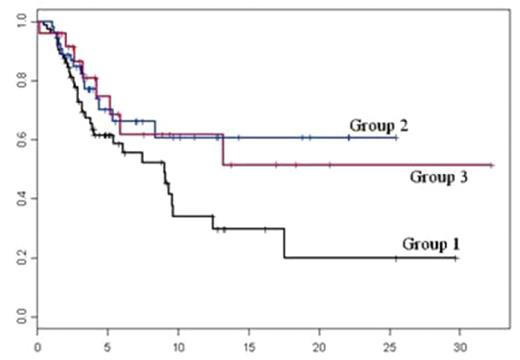
This analysis concerned 164 allogeneic HSCT after standard (Std) or reduced intensity conditioning (RIC) using double cord blood cells (CBC), reported to the SFGM-TC registry. There were 57 females (F) and 107 males (M) with a median age of 39.5 years (18–66). The diagnosis pretransplant were acute leukaemia: 93 (56 AML and 37 ALL), MDS: 9, MPS: 9 (CML: 4), CLL: 5, NHL: 18, HD: 7, MM: 13, AA: 7, other diseases: 3 (2 inborn errors and 1 solid tumour). The median interval between diagnosis and HSCT was 20.6 months (2.6–385.5). Among 154 evaluated patients (pts), disease status prior conditioning were 92 CR (CR1: 45, CR 2: 34, >CR2: 12 and 1 non classified), 21 PR, 21 stable diseases (SD) (SD: 6, AA: 6, inborn errors: 2, CML in CP: 3, myelofibrosis: 2 and MDS: 2), 22 progressive diseases (PD) (PD: 4, relapses: 10 and refractory diseases: 8), 8 pts were not documented. Among 158 pts documented, 49 (31%) were completely sex matched and 109 (69%) sex mismatched [72 CBC1+2 (F+F or F+M) for a M recipient and 37 CBC1+2 (M+M or M+F) for a F recipient]. Among 158 documented, 42% of recipients, 37% of CBC1 and 38% of CBC2 were CMV+; there was a complete ABO compatibility between the 2 CBC and the recipient in 38 cases, 1 or 2 minor incompatibilities in 40 cases and almost 1 major incompatibility in 80 cases. For HLA matching, we distinguished 3 groups: group1 [n=78 (HLA compatibility at least 4/6 between recipient and CBC1+2) and between CB1 and CB2 including total HLA DRB1 matching)], group 2 [n=55 (HLA compatibility at least 4/6 between recipient and CBC1+2) considering neither HLA compatibility between CBC1-CBC2 nor HLA DRB1 matching)] and group3 [n=25 (all others)]. At harvesting, the median number of total nucleated cells (TNC) (x107/kg) was 4.67(1.6–12.2), the CD34+ (x105/kg) 1.8 (0.3–10.8), the CFU-GM (x104/kg) 3.67 (0.94–25), and after thawing 3.24(0.58–12), 1.4(0.2–9.2) and 2(0.27–16.4) respectively. The TNC threshold number was set to 5x107/kg because more than 96% of pts received more than 3x107/kg. Among 135 documented, 26 (19%) received Std conditioning and 109 (81%) RIC. After transplantation, 129 pts (96%) engrafted with 86% (80–92) of neutrophil recovery at day 60 with no significant difference according to TNC (<5x107/kg: 88%, ≥ 5 x107/kg: 90%; p=0.28) and HLA matching (group1: 86.6%, group2: 89.6% and group3: 83.3%; p=0.81). Eighty-four pts developed an AGVHD: gr I: 20 and ≥ gr II: 60 (35 gr II, 16 gr III and 4 grade IV), 4 patients were not classified. At day 90, the cumulative incidence of AGVHD grI was 10.4%(5–16), gr ≥ II: 42%(33–51)[grII: 24%(16.5–32), grIII-IV: 18%(11–25)]. Moreover, we observed for AGVHD gr ≥ II according to HLA typing and TNC: group1: 41%(28–54), group2: 46%(31–60) and group3: 33%(8–58); TNC<5x107/kg: 38%(25–51) and TNC>5.107/kg: 46%(32–60). Twenty-one pts presented a chronic GVHD (9 limited and 12 extensive) and the cumulative incidence at 1 year was 13.7%(4–24) for limited and 20%(9–21) for extensive. With a median follow-up of 7.3 months, the probability of 1-year and 2-year overall survival and disease-free survival were 49.6% (40–61.5) and 38% (27–54), 43% (33.5–54.5) and 36% (25–51) respectively. The probabilities of OS, NRM and RM according to TNC, disease status pre-transplant, HLA matching and sex matching are shown in Figure 1 and Table1.The multivariate analysis showed a significant impact of 2 factors on OS: disease status PD vs CR: HR=6.16 (1.87–20.25) (p=0.002); HLA matching group2 vs group1: HR=0.29 (0.11–0.82) (p=0.01), and 3 significant factors on DFS: sex-matched HR=0.29 (0.09–0.94) (p=0.03), sex-mismatched (F recipient) HR=0.15 (0.04–0.61) (p=0.008) and HLA matching (group 2 vs group1) HR=0.32(0.11–0.88) (p=0.02).A refined chimerism analysis is ongoing and will be presented. In conclusion, this large retrospective analysis showed that the quantitative objective of double cord blood use for allogeneic HSCT is achieved (only 4% had received < 3x107/kg TNC) with no further significant impact of TNC number on OS, NRM and RM. As usual in other types of allogeneic HSCT, we demonstrated the significant impact of disease status before transplantation on transplant outcome. Finally, the most interesting point was the better results observed in group 2 but which needs more precise analysis in the future.
Table 1. Probability of OS, NRM, RM according to different variables.
| . | Probability of OS . | Probability of NRM . | Probability of RM . |
|---|---|---|---|
| Whole population (cummulative 1 year) | 49.6%(40–61.5) | 49.7%(39–60) | 7.5%(2–17) |
| TNC | |||
| TNC < 5 × 107/kg | 50%(36.6–68.5)) | 47%(32–62) | 8%(0–16) |
| TNC ≥ 5 × 107/kg | 44.5%(29.6–67) | 56.5%(38.5–74.5) | 9.5%(0–20) |
| Disease status pre-transplant | |||
| CR | 51%(38–68) | ||
| PR | 54%(31–92.5) | ||
| SD | 75%(43–100) | ||
| PD relapse | 35.5%(18–70) | ||
| HLA compatibility | |||
| Group 1: 4/6 or more for all(2/2 for DRBI) | 34%(21–54) | 62%(46–78) | 10%(3–20) |
| Group 2: 4/6 or more for R-CB1 and R-CB2 | 61%(45–81) | 39%(21–57) | 2%(0–6) |
| Group 3: Others | 61.6%(42–90) | 42.5%(19–66) | 10%(0–24.5) |
| Sex matching | |||
| M recipient with sexmismatch | 35%(22–57) | 63%(46–79) | 8%(2–14) |
| Sexmatch | 61%(45–82) | 43%(23.5–63) | 4.5%(0–13.5) |
| F recipient with sexmismatch | 54%(36.5–80)) | 42%(24–62) | 9%(0–22) |
| . | Probability of OS . | Probability of NRM . | Probability of RM . |
|---|---|---|---|
| Whole population (cummulative 1 year) | 49.6%(40–61.5) | 49.7%(39–60) | 7.5%(2–17) |
| TNC | |||
| TNC < 5 × 107/kg | 50%(36.6–68.5)) | 47%(32–62) | 8%(0–16) |
| TNC ≥ 5 × 107/kg | 44.5%(29.6–67) | 56.5%(38.5–74.5) | 9.5%(0–20) |
| Disease status pre-transplant | |||
| CR | 51%(38–68) | ||
| PR | 54%(31–92.5) | ||
| SD | 75%(43–100) | ||
| PD relapse | 35.5%(18–70) | ||
| HLA compatibility | |||
| Group 1: 4/6 or more for all(2/2 for DRBI) | 34%(21–54) | 62%(46–78) | 10%(3–20) |
| Group 2: 4/6 or more for R-CB1 and R-CB2 | 61%(45–81) | 39%(21–57) | 2%(0–6) |
| Group 3: Others | 61.6%(42–90) | 42.5%(19–66) | 10%(0–24.5) |
| Sex matching | |||
| M recipient with sexmismatch | 35%(22–57) | 63%(46–79) | 8%(2–14) |
| Sexmatch | 61%(45–82) | 43%(23.5–63) | 4.5%(0–13.5) |
| F recipient with sexmismatch | 54%(36.5–80)) | 42%(24–62) | 9%(0–22) |
Probability of OS according to different HLA groups
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal