Abstract
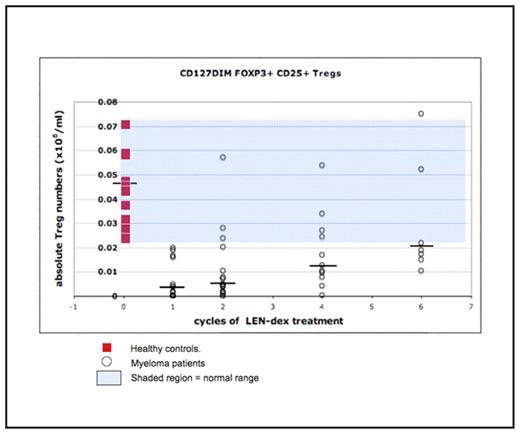
CD4+CD25+Foxp3+ regulatory T cells (Tregs) are a group of immune-suppressive T cells responsible for the maintenance of self-tolerance and autoimmunity. Increased Tregs have been implicated in suppression of tumour-immunity, and are associated with poor prognosis in gastric, oesophageal and ovarian cancers. Conversely, reduced Tregs are associated with aggressive disease and poor prognosis in lymphoproliferative disorders such as follicular lymphoma and Hodgkin lymphoma. Meanwhile, conflicting literature exists with regards to the role of Tregs in the pathogenesis of multiple myeloma (MM). Lenalidomide (LEN) is an immunomodulatory drug (ImiD™) that increases T cell numbers and function in vitro but the impact on Tregs in vivo is unknown. As part of an ongoing clinical trial of low-dose lenalidomide, peripheral blood lymphocyte subsets (LSS) and Treg numbers were examined in patients [n=18, median age 67 years (49–77)] with relapsed/refractory MM at baseline and at various time points during treatment with combination LEN (15mg/o/d d1–21q28)-dexamethasone (dex) (20mg/o/d d1–4,9–12,17–20 q28), in order to measure changes induced by LEN-dex treatment. Results were compared to 10 age matched healthy donors. LSS and Tregs were assessed by flow cytometry, with Tregs strictly defined as CD4+CD25hiCD127dimFOXP3+. At baseline, MM patients had depressed B cells (median 0.76 vs. 3.2 ×105/ml; p=0.02) and CD3+ T cells (median 7.2 vs. 12.1 ×105/ml; p<0.001) compared to healthy donors, with an inverse CD4:CD8 T cell ratio (0.7:1 vs. 2.9:1, p=0.008). Tregs in MM patients were markedly reduced at baseline compared to healthy donors [median 0.40 (range: <0.01–1.9) vs. 4.8 (range 2.4–7.1) ×104/ml; p=0.0005]. In 11 patients completing at least 4 treatment cycles, no recovery of B cells (7.6 vs. 2.3 ×105/ml, p=0.053), NK cells (2.1 vs. 2.7×105/ml, p=0.1) or T cells (5.6 at baseline vs. 7.5 × 105/ml, p=0.45) were seen despite all achieving at least a PR (one with IF negative CR). In contrast, median Treg numbers progressively increased towards normal range, from a baseline of 0.3 to 1.3 × 104/ml (p=0.005) and 2.0 × 104/ml (p=0.009) after 4 (n=11) and 6 (n=7) cycles of LEN-dex respectively (figure 1). Patients with relapsed/refractory MM have profoundly disturbed LSS including marked decreased in Treg numbers. Normalisation of Treg numbers in responding patients treated with LENdex suggest that, as in other tumours, Tregs are actively involved in the pathophysiology of MM and their modulation may be an important component of the immunomodulatory mechanisms of LEN.
Change in regulatory T cell (Treg) numbers with each cycle of LEN-dex in MM patients
Change in regulatory T cell (Treg) numbers with each cycle of LEN-dex in MM patients
Disclosures: Lynch:Celgene Pty Ltd.: Employment.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal