Abstract
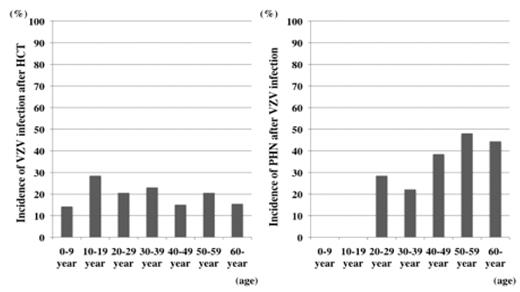
Reactivation of varicella-zoster virus (VZV) is a common event in patients undergoing hematopoietic cell trasnplantation (HCT). In post HCT recipients, VZV reactivation can occur frequently as localized zoster and sometimes as disseminated cutaneous lesions resembling varicella with or without visceral involvement, which results in a high mortality rate. The most common complication associated with zoster in healthy individuals is chronic and often debilitating pain called post-herpetic neuralgia (PHN), which can last for several yeas and may reduce quality of life. Although, many previous studies have shown a high incidence of VZV reactivation after HCT, incidence and risk of PHN in HCT recipients have not yet been clarified. To assess the incidence and risk factors associated with PHN after post-HCT VZV infection, we conducted a retrospective chart review of 418 consecutive patients who underwent HCT in Hokkaido Cooperative Hematology Group (HCHG) between April 2005 and March 2007. HCHG is multicentric clinical study group that includes “all” hematology departments in Hokkaido prefecture, consisting of 26 clinical groups of 19 institutes. VZV infection was defined by the appearance of typical cutaneous vesicular lesions or the detection of VZV antigen. Localized zoster was defined as the presence of vesicular lesions in a dermatomal distribution. Disseminated zoster was defined as a generalized vesicular eruption that is identical to that of varicella. Visceral dissemination was defined as clinical evidence of internal organ involvement in the absence of other identified pathogens that might have accounted for the clinical syndrome. Post-herpetic neuralgia was defined as dermatomal pain that persisted beyond rash healing. Information on pre-transplant therapeutic exposures, HCT procedures and post-transplant health complications was obtained via evaluation form. A total of 418 patients were included in this study. Male/Female ratio was 221/197, median age at HCT was 47 years (range, 0–69 years), autologous HCT/allogeneic HCT/syngeneic HCT ratio was 154/263/1, and median length of follow-up was 344 days (range, 3–1165 days). Seventy-eight patients developed VZV infection after HCT (M/F=36/42; median age, 48 (range, 3–68) years; auto/allo/syngeneic=29/48/1). Sixty-two patients had localized zoster (single dermatome in 53, double dermatome in 9), 12 patients had disseminated zoster (rash like chicken pox), and 4 patients had visceral zoster (involvement of GI the tract). All cases were treated by ACV or VACV, and there was no VZV infection-related death. After resolution of VZV infection, VZV infection reoccurred in 5 cases (localized zoster in 4 cases and visceral zoster in 1 case). Cummulative incidences of VZV infecion in allo-HCT and auto-HCT recipients were estimated to be 34% and 22%, respectively, at 2 years after HCT. In autologous HCT, 96.6% of the cases of VZV infection occurred during the first year after HCT, but in allogeneic HCT, only 75.5% of the cases of VZV infection occurred during the first year after HCT. Twenty-seven (35%) of the 78 patients with VZV infection suffered PHN after resolution of VZV infection (M/F=15/12; median age, 56 (range, 21–64) years; auto/allo=13/14). Although incidences of VZV infection were not different between age groups, the incidence of PHN increased with advance of age (Figure). In HCT recipients, the incidence of PHN increased at a younger age than that in healthy individuals. Multivariate analysis showed that advanced age (P=0.0031; OR=1.09; 95% CI, 1.03 to 1.15) and male gender (P=0.046; OR=3.09; 95% CI, 1.02 to 9.35) were associated with increased risk of PHN. Auto vs allo, CST vs RIST, and onset of VZV infection after HCT were not significant. In allogeneic HCT recipients, existence of GVHD at onset of VZV infection and prophylaxis of GVHD with tacrolimus were associated with increased risk of PHN in univariate analysis, but these factors were not significant in multivariate analysis. This study showed the magnitude of risk of PHN in HCT recipients and revealed advanced age and male gender to be risk factors, suggesting the usefulness of acyclovir as prophylaxis for prolonged periods in these patients.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal