Abstract
In order to determine the long-term impact of AUTO in patients (pts) with T-cell lymphoma, we examined the outcome of 79 pts transplanted at the MD Anderson Cancer Center, in first partial or complete remission (CR) (AUTO1, n=20) or for relapsed / refractory disease (AUTO2, n=59) between 06/91 and 05/08.
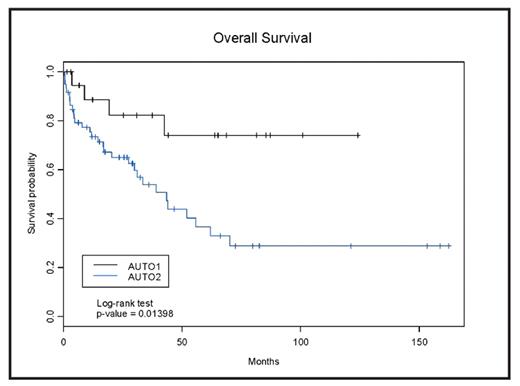
<<<PATIENTS>>> Median age (range) at transplantation was 49 (22–65) and 51 (16–77) for the AUTO1 and AUTO2 groups respectively (p=0.35); other baseline characteristics including gender, stage, B-symptoms, LDH, IPI, PET/Gallium status, history of marrow involvement, and performance status at transplantation were similar. There was a statistically significant difference between AUTO1 and AUTO2 with respect to histology {peripheral t-cell, angioimmunoblatic, and anaplastic/large cell were present in 80%, 5%, 15%, respectively in AUTO1, and 42%, 10%, and 45%, respectively in AUTO2 (p=0.02); one pt in AUTO2 had small lymphocytic and one had hepatosplenic T cell lymphoma}. Statistically significant differences were also noted with respect to B2-microglobulin (P=0.02; favoring AUTO1), number of prior chemotherapy regimens received {median 1 vs 3 for AUTO1 and AUTO2, respectively (p <0.001)}, disease status at transplantation {18% of AUTO2 had stable or progressive disease at transplant vs 0% in AUTO1 (P < 0.001)}, and # of CD34+cellsx10 6/Kg infused {median 9 vs 5 for AUTO1 and AUTO2, respectively}. Most pts in both group received BEAM as conditioning. Median follow-up time in months was 64 (95%CI, 31–87), and 47(95%CI29–121) for AUTO1 and AUTO, respectively. Median overall survival (OS) was 43.5 months (95%CI:30–70 for AUTO2 and the median OS was not reached for AUTO1 (P=0.01)(Figure). The median progression-free survival (PFS) was 16 months (95%CI:8–56) and 95 months (95%CI:6.94-NA) for the pts in the AUTO2 and AUTO1 groups, respectively (P=0.06). Univariate Cox models for OS showed that AUTO2 vs AUTO1 (HR 3.4, P=0.02), high LDH level (HR 2.6. P=0.01), PET/Gallium+ (HR 2.8, P=0.01), IPI2–4 (HR 3.4, P=0.002), marrow involvement (HR 6.3, P=0.02), and marrow vs peripheral blood as source of graft (HR 2.1, P=0.048) were important determinants of outcome. The univariate Cox model for PFS showed that only AUTO2 vs AUTO1, hi LDH, IPI and PET/gallium were statistically significant. A multivariate analysis that included the covariates with the lowest P value showed that AUTO2 vs AUTO1 remained the only important factor for OS (HR 4.79, P=0.035) while PET/ Gallium status at transplantation was the most important determinant of PFS (HR 3.13, P=0.006).
<<<CONCLUSION>>> Autologous transplantation has the potential to cure a proportion of pts with t-cell lymphoma if performed during the first remission. Alternative strategies are needed for pts transplanted beyond first remission especially if they continue to have avid functional imaging at transplantation.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal