Abstract
BACKGROUND: Many recent advances have occurred in the field of MDS including hypomethylating agents, lenalidomide, and WHO classification. Likewise the field of HCT has also undergone major new developments including non ablative conditioning, better supportive care, better HLA typing, selection of unrelated donors and development of reduced toxicity ablative regimens like Busulfan and Fludarabine. The role of HCT therefore needs to be redefined in light of these developments. The purpose of this study is to report our recent results.
PATIENTS AND METHODS: 89 consecutive patients with MDS as defined by WHO criteria treated at our institution between Jan 2002 and April 2008 are included in this report. There were 60 males and 29 female with a median age of 54 (23–67). There were 5(6%) patients with RA, 1(1%) RARS, 9(10%) RCMD, 22(25%) RAEB 1, 17(19%) RAEB 2, and 35(39%) therapy related MDS(t MDS). Their IPSS scores were 25(28%) patients with Intermediate 1, 49(55%) Intermediate 2, 15(17%) high. Their WPSS categories were 5(6%) patients Low, 9(10%) Intermediate, 49(55%) high, and 26(29%) very high. 51(57%) patients had a matched related donor and 38(43%) had an unrelated donor. Conditioning regimen were Flu/Bu in 56(63%) patients, Bu/Cy 1(1%), Flu/Mel 32(36%). According to HCT-CI index, the comorbidity scores were 0 in 16(18%) patients, 1 or 2 in 19(21%) and greater then 2 in 54(61%). Median time from diagnosis to transplant was 8 months (range 1–51 months).
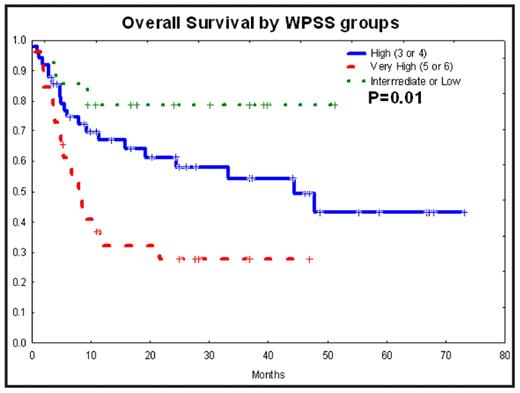
RESULTS: With a median follow up of 28 (3–73) months, 2 year overall(OS) and disease free survival were 54%(95% CI; 42%–66%) and 52%(95% CI; 40%–64%) respectively. Cumulative incidence of non relapse mortality at 2 years was 23% (95% CI; 16%–35%). Cumulative incidence of relapse mortality at 2 years was 23% (95% CI; 15%–34%). As per WHO grouping, OS was 63%, 60%, 46% and 48% in patients with Low blast count (RA, RARS, RAMD), RAEB1, RAEB2 and t MDS( p=0.46) respectively. WPSS score was significantly(P=0.01) predictive of overall survival (see fig): 27% surviving in very high risk group, 61% in high risk group and 78% in Low and intermediate risk group. Likewise cytogenetic risk group and IPSS were significantly predictive of survival. Donor type or graft source did not predict outcome. Five patients developed primary(3) or secondary(2) graft failure. Median time to neutrophil engraftment was 13 days (8–26 days) and to platelet engraftment was 16 days (9–89 days).
CONCLUSION: These results in patients with comorbidities and with a median age of 54 years are promising. Cytogenetics and prognostic scores based on cytogenetics predict outcome after HCT.
Disclosures: Jones:Otsuka: Membership on an entity’s Board of Directors or advisory committees. Andersson:PDL Biopharma: Consultancy.
Author notes
Corresponding author

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal