Tosetto and colleagues have developed a mathematical method to quantify the odds of having type 1 von Willebrand Disease based on a person's family history, bleeding score, and VWF level.
Accurate diagnosis of type 1 von Willebrand disease (VWD) remains a clinical challenge. In many instances, there is great overlap between VWD patients and normal individuals in both clinical and laboratory outcomes.1 To address these difficulties, provisional diagnostic criteria established by experts focus on 3 components of disease: (1) presence of bleeding symptoms, (2) reduced von Willebrand factor (VWF) levels, and (3) autosomal inheritance of the phenotype.2 In this issue of Blood, Tosetto and colleagues have developed a novel method that allows for a more rigorous, quantitative analysis of the relative contribution of these 3 components to the odds of having VWD.
In the general population, prevalence estimates of VWD range from 0.1% to 1%, meaning that a random person would have a 0.1% to 1% chance of having VWD.3,4 Intuitively, gathering more information about the person (such as bleeding score) changes one's estimation of his or her probability of having VWD. In their study, Tosetto and colleagues have translated this intuitive concept into a mathematical model. Based on the Bayes theorem, their algorithm utilizes clinical and laboratory phenotypes to update individual odds of having VWD. Statistically speaking, population prevalence serves as the prior estimate of disease that is multiplied by likelihood ratios (LRs) for specific outcomes to obtain a person's final odds of having the disease.
Corresponding to the clinical definition of disease and to the 3 components of the provisional diagnostic criteria, Tosetto and colleagues have defined 3 informative LRs for assessing disease odds: an LR based on bleeding score, an LR based on VWF level, and an LR based on family history of disease. Although their methods are theoretically sound, the strength of their results hinges on the appropriateness of the populations used to derive these likelihood ratios. To retain multiplicative properties of the method, the 3 populations must be independent from each other (for example, platelet function analyzer [PFA-100TM; Dade Behring, Deerfield, IL] values cannot determine an independent LR because they are directly correlated with VWF levels). Tosetto and colleagues provide good arguments for the use of their populations, but also recognize the need for verifying LR estimates with other populations.
Results reported by Tosetto and colleagues offer important insights into VWD diagnostic difficulties. First, none of the 3 criteria alone results in odds of disease over 2.0—indicating that at least 2 positive findings are needed to diagnose disease. Second, based on magnitudes of LRs, family history serves as the most important diagnostic criteria, followed by VWF levels and then by bleeding symptoms. However, because LRs for VWF and bleeding symptoms are derived from VWD cases selected on the basis of family history, the importance of family history may be slightly elevated in this study. Lastly, the investigators' results identify specific situations in which use of the provisional criteria for disease diagnosis is more likely to result in disease misclassification. While this study's results should be validated, the authors' Bayesian method for diagnosing type 1 VWD shows promise as a valuable tool to aid clinical diagnosis of disease.
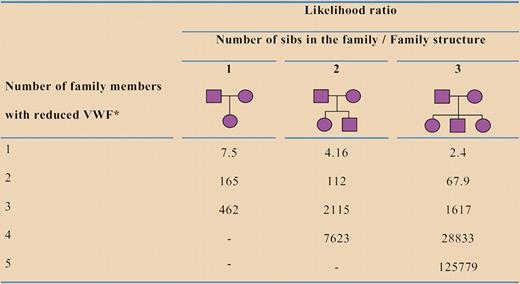
Likelihood ratios for VWD in a nuclear family, based on the number of siblings in the family and on the number of family members with reduced VWF levels (below the 25th percentile). *Including propositus. See the complete figure in the article beginning on page 3998.
Likelihood ratios for VWD in a nuclear family, based on the number of siblings in the family and on the number of family members with reduced VWF levels (below the 25th percentile). *Including propositus. See the complete figure in the article beginning on page 3998.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal