Traditionally, neutrophils and neutrophil-derived enzymes have been viewed to play a role exclusively in host defense. However, there is growing evidence that neutrophils also contribute to the regulation of vascular tone.
In mediating host-defense reactions, circulating polymorphonuclear neutrophils (PMNs) adhere to endothelial cells, extravasate, phagocytose invading pathogens, and release a noxious collection of bactericidal effector molecules into phagolysosomes. One aspect of this armamentarium is PMN expression of enzymes that produce a variety of reactive oxygen species (ROS), including NADPH oxidase and myeloperoxidase. Upon activation, the “respiratory burst” induced by the assembly and activation of NADPH oxidase subunits produces superoxide (O2−) and its dismutation product, hydrogen peroxide (H2O2). In concert with this, the heme center of myeloperoxidase (MPO) reacts with H2O2 to form a more potent oxidizing intermediate that, in turn, oxidizes chloride (Cl) to yield hypochlorous acid (HOCl). The concerted reactions of these species induce the oxidation of a multitude of biomolecules that results in the destruction of the pathogen, and sometimes, unfortunate collateral damage to the host.
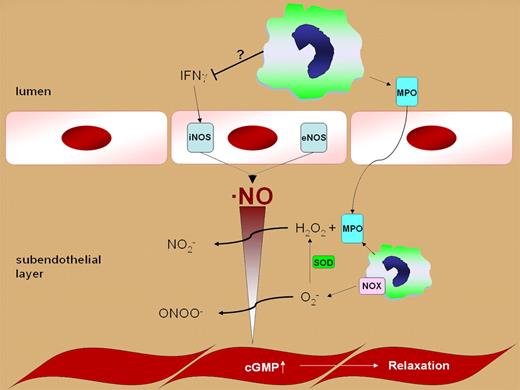
Regulation of vascular NO homeostasis by polymorphonuclear neutrophils.
Regulation of vascular NO homeostasis by polymorphonuclear neutrophils.
Recently, there has been growing evidence revealing that PMN-derived pro-oxidative enzymes not only mediate acute inflammatory responses, but also contribute to the pathogenesis of diseases associated with chronic inflammation, including atherosclerosis, asthma, Alzheimer's disease, and cancer.1 Of relevance, it has been shown that endothelium-derived nitric oxide (NO) is catalytically consumed by NADPH oxidase and MPO-dependent reactions, resulting in impaired endothelial function and the formation of secondary oxidizing and nitrating species.2 These reactions can also occur at anatomic sites remote from activated PMN upon the release of MPO during PMN degranulation and transcytosis of free MPO into the vessel wall and subendothelial matrix. In aggregate, activated PMNs are typically viewed to manifest redox reactions and secondary inflammatory mediators that conspire to not only serve a host defense role, but also impair vascular function.
In this issue of Blood, Morton and colleagues make the landmark observation of a new physiologic function of neutrophils—the regulation of vascular tone in vivo. They show that depletion of neutrophils in healthy mice leads to a reduction in systolic blood pressure and an impairment of vascular constriction studied ex vivo. They attribute this effect to neutrophil suppression of interferon-γ (IFNγ)–mediated inducible nitric oxide synthase (iNOS) expression. However, involvement of bacteria-derived stimuli cannot be excluded, because treatment with enrofloxacin partially inhibited the hypotension induced by neutropenia.
The possibility that the neutropenic mice might be prone to development of low-grade inflammation is a limitation for this murine model. However, the absence of elevated LPS levels and an absence of most commonly occurring microbial pathogens strongly supports the conclusion that there is a pathogen-independent effect of neutrophils on blood pressure regulation. In this context, potential off-target, non-antimicrobicidal effects of enrofloxacin might also need to be considered. Furthermore, it has to be pointed out that, while IFNγ has been identified as a critical mediator for iNOS expression, detailed signaling mechanisms linking neutropenia, IFNγ, and iNOS remain to be defined.
The important aspect of this study is the novel observation that under basal conditions, neutrophils are poised to exert host-defense–related inflammatory responses and are also contributing to the physiological regulation of blood pressure. This observation allows exciting new perspectives about how neutrophils function in vivo, and should motivate more detailed future investigation of the signaling events that link bacterial surveillance by neutrophils in healthy individuals, the maintenance of normal vascular homeostasis, and responses to both neutropenia and various inflammatory stimuli. It is likely that further study will reveal interesting linkages between neutrophil-derived reactive species, redox-dependent cell-signaling pathways, and downstream transcriptional regulation of expression of key gene products.
Conflict-of-interest disclosure: The authors declare no competing financial interests. ■

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal