Abstract
Accurate estimation of risk for venous thromboembolism (VTE) may help clinicians assess prophylaxis needs. Only empirical algorithms and risk scores have been described; an empirical risk score (‘Kucher’) based on 8 VTE risk factors (cancer, prior VTE, hypercoagulability, surgery, age>75 yrs, BMI>29, bed rest, hormonal factor) using electronic alerts improved hospitalized patient outcome (
NEJM 2005;352:969–77
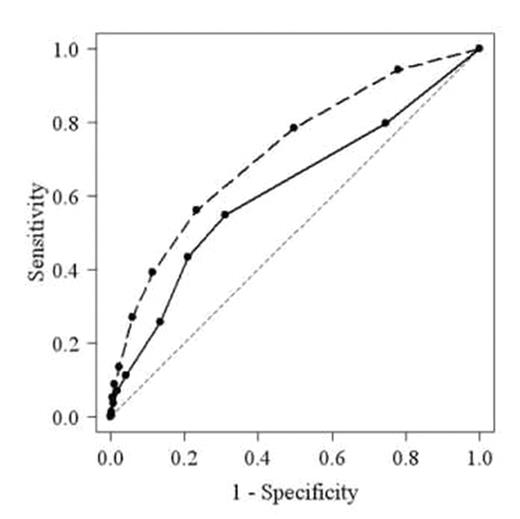
). We wished to develop a multivariate regression model for VTE risk, based on Kucher, and validate its performance. The initial derivation cohort consisted of patients enrolled in ‘VERITY’, a multicentre VTE treatment registry for whom the endpoint of VTE and all 8 risk factors were known. Initial univariate analysis (n=5928; 32.4% with diagnosis of VTE) suggested VTE risk was not accounted for by the 8 factors; an additional 3 were added (leg paralysis, smoking, IV drug use [IVD]). The final derivation cohort was 5241 patients (32.0% with VTE) with complete risk data. The validation cohort (n=915) was derived from a database of 928 consecutively enrolled patients at a single DVT clinic. Model parameters were estimated using the statistical package ‘R’ using a stepwise selection procedure to choose the optimal number of main effects and pair-wise interactions. This showed that advanced age (estimated odds ratio [OR]=2.8, p<0.001); inpatient (OR=3.0, p<0.001); surgery (OR=3.1, p<0.001); prior VTE (OR=2.9, p<0.001); leg paralysis (OR=3.8, p<0.001); cancer (OR=5.3, p<0.001); IVD (OR=14.3, p<0.001); smoking (OR=1.2, p=0.009); and thrombophilia (OR=2.8; p<0.001) increased the risk of VTE. Obesity (OR=0.7; p<0.001) increased the VTE risk only in patients with a hormonal factor (OR=2.0, p=0.007). Backward stepwise regression showed prior VTE as the most important factor followed by cancer, IVD, surgery, inpatient, age, leg paralysis, hormonal factor, obesity, thrombophilia and smoking. Expressing the parameter estimates in terms of probabilities defines a risk score model for VTE. Using the model, the receiver operating characteristic (ROC) curve (see figure) area under the curve (AUC) was estimated as 0.720 (95% CI, 0.705–0.735) for the model (dashed line), indicating a good diagnostic test significantly better (p<0.001) than Kucher (AUC=0.617, 95% CI, 0.599–0.634)(solid line). For the validation cohort, AUC was estimated as 0.678 (95% CI, 0.635–0.721) for the model, which was not significantly different from AUC for the full dataset used for model development, and was 0.587 (95% CI, 0.542–0.632) for Kucher. This model to predict individual patient risk of VTE may contribute to decision making regarding prophylaxis in clinical practice.Author notes
Disclosure: Consultancy: MMRx and University of Warwick have provided consultancy services to sanofi-aventis. Research Funding: The VERITY registry is supported by an unrestricted edcuational grant by sanofi-aventis.
2007, The American Society of Hematology
2007

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal