Abstract
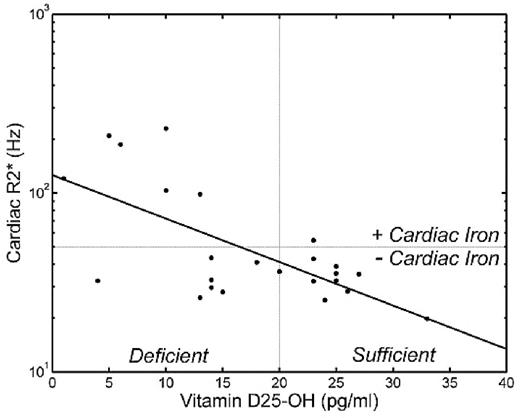
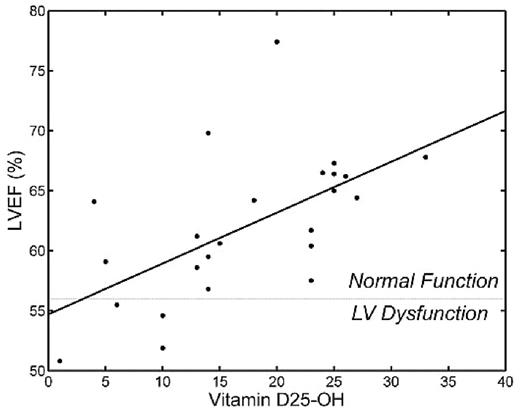
Vitamin D deficiency is epidemic in the United States and is associated with decreased calcium absorption and metabolism, leading to bone loss, muscle weakness, and impaired pancreatic function. Many thalassemia major patients, as a result of decreases sunlight exposure and increased metabolic demand, are vitamin D deficient. We hypothesized that vitamin D deficiency might be associated with cardiac siderosis and impaired cardiac function through its modulation of calcium signaling in these patients. Methods: Permission for review of medical records was obtained from the Committee on Clinical Investigation at Children’s Hospital Los Angeles. We compared vitamin D25-0H and D1-25 levels in our thalassemia major patients with cardiac R2* (1/T2*) and left ventricular ejection fraction (LVEF) from the patient’s most recent cardiac MRI. Time difference between the exams was 2.8 ± 3.3 months with a range of 0.2 to 9.4 months. Other parameters recorded included age, gender, ferritin, liver iron (by MRI) and transferrin saturation. Univariate and multivariate regression was performed using JMP 5.1 (SAS, Cary, NC). Results: Twenty four patients had records suitable for review. There were 11 women and 13 men with a mean age of 14.7 ± 7.6 years [1.4 – 25.8]. Population was moderately iron overloaded with ferritin values of 2089 ± 1920 ng/ml [246 – 8230], liver iron 13.7 ± 11.4 mg/g dry wt [2–39.5], cardiac R2* 65 ± 61 Hz [19.8 – 229], and transferrin saturation 84 ± 18% [36%–106%]. Vitamin D25-OH levels were markedly depressed, 17.1 ± 8.5 pg/ml [1–33], with 13/24 values below the lower limit of 20 ng/ml. Surprisingly, vitamin D1-25OH levels were normal or elevated in all patients, 59.9 ± 19.5 pg/ml [32–103] with four patients exceeding the upper limit of normal of 71 pg/ml. There was no correlation between D25-0H and D1-25OH levels. D25-OH levels (but not D1-25OH levels) fell sharply with age (r2 = 0.48) and were negatively associated with liver iron (r2 = 0.20). Figures 1 and 2 demonstrated cardiac R2* and LVEF as functions of D25-OH levels. Cardiac R2* was log-linearly correlated with D25-OH level (r2 = 0.44, p=0.0001; levels below 13 ng/ml were associated with severe cardiac iron loading. Multivariate analysis of D25-OH, D1-25, HIC, ferritin, age, and transferrin saturation demonstrated that D25-0H and ferritin are the sole predictors of abnormal cardiac R2*, accounting for 38% and 5% of the variability respectively. LVEF was also negatively related to D25-OH levels (r2 = 0.35, p = 0.002). In multivariate analysis, vitamin D250H and vitamin D1-25OH levels accounted for 50% of the LVEF variability, independent of cardiac R2*. Conclusion Vitamin D deficiency is common in thalassemia major patients and strongly associated with cardiac iron uptake and ventricular dysfunction.
Author notes
Disclosure:Consultancy: Dr. Wood and Dr Coates have served as consultants to Novartis. Research Funding: Dr. Wood and Dr. Coates have received research funding from Novartis and from Apotex. Honoraria Information: Dr. Wood has received honoraria from Novartis and from Apotex. Dr. Coates has received honoraria from Novartis. Membership Information: Dr. Wood is an advisor to the Exjade Speakers Bureau. Dr. Coates participates in the Exjade Speakers Bureau. Off Label Use: Cardiac T2* measurements are not FDA approved.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal