Abstract
Background: For all “transplant eligible” pts with MM, established practice guidelines recommend ASCT as part of the front line treatment. However, the definition of “transplant eligible” remains undefined. The HCT-CI is a new tool that encapsulates pre-transplant comorbidities used in predicting transplant outcomes in pts undergoing allogeneic SCT. This scoring system has been shown to be a good predictor for non-relapse mortality (NRM) & survival in pts undergoing alloSCT. In this study, we hypothesize that HCT-CI could predict the transplant outcome on pts with MM undergoing ASCT and could potentially be utilized as a tool for selecting pts with MM for transplant.
Methods: A retrospective analysis of 75 pts with multiple myeloma whom underwent ASCT in our institution between 02/99 and 12/03 with a median follow up of 30 months. Pts were assigned scores based on the HCT-CI. Definitions of comorbidities were as previously reported by
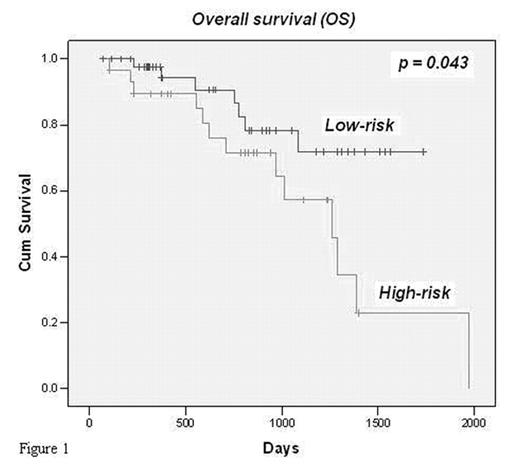
Results: Median age was 56 years (38 – 73); M:F 1:1. 51 pts received a single & 24 had tandem ASCT. The majority of pt. had IgG myeloma (IgG kappa: 45; IgG Lambda 17). Comorbidities (points, number of pts): mild hepatic (1,16), renal (2,6), cardiac (1,8), arrhythmia (1,1), heart valve disease (3,4), cerebrovascular (1,8), DM (1,11), PUD (2,2), inflammatory bowel disease (1,0), Tumor (3,6), pulmonary (2,5), psychiatric (1,8), rheumatologic (2,3), infection (1,6), and obesity (1,10). HCT-CI score of 0 seen in 32%, 1 in 28%, 2–8 in 40% of the pts, with a median score of 1.65. 20 patients died with only one due to NRM. Pts were categorized into 2 groups: low-risk (scores of 0–1) – 46 pts and high-risk (scores 2–8) – 29. Using a cox regression model, the low risk group had a survival advantage (HR = 2.55, P = 0.04). Using Kaplan Meier survival estimate comparing the low risk and high risk group (figure1), the 5 yrs overall survival were 77% & 22% respectively (P = 0.04). While the median survival for the high risk group was 3.52 years, it has not been reached for the low risk group.
Conclusion: Here, we have demonstrated a survival benefit for pts with low (0–1) compared with high (≥ 2) HCT-CI score. In addition, the outcome of pts with high HCT-CI score was also similar to non-transplant pts as published in the literature. This raises the question of “benefit” of ASCT for pts with high HCT-CI score. Thus, HCT-CI may serve as a useful tool to select pts whom would benefit most from ASCT.
Figure 1
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal