Abstract
PURPOSE: To examine the value of allogeneic HCT in the treatment of therapy-related myelodysplastic syndrome/acute leukemia (t-MDS/t-AL) which develops after previous exposure to chemotherapy (CT) or radiotherapy (RT), we retrospectively analyzed the data of 47 patients who were treated at our institution between 1996 and 2007.
PATIENTS AND METHODS: The primary diseases included malignant lymphoma (n=17), breast cancer (n=13) and other solid tumors (n=17) which had been treated with various cytotoxic drugs including alkylating agents (n=30), topoisomerase II inhibitors (n=22), and/or RT (n=20). The median interval between the diagnosis of the primary disease and the onset of t-MDS/t-AL was 3.8 years (range, 0.8–18.9). Twenty-five patients had AML, 5 ALL, 1 biphenotypic acute leukemia, and 16 MDS. Cytogenetic risks were assigned according to the SWOG criteria for AML patients. ALL patients with a normal karyotype were categorized in the intermediate group, and those with t(9;22) or t(4;11) were in the unfavorable risk group. MDS patients without progression to AL were categorized into the favorable risk group.
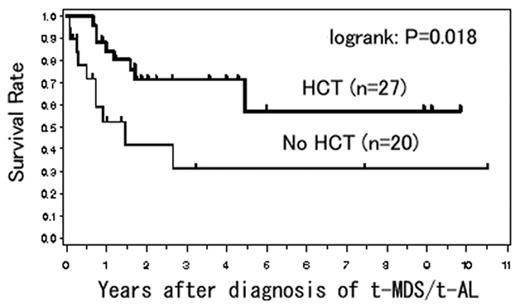
RESULTS: Thirty-three patients received disease-adapted CT, with a response rate of 73%, while 14 patients were elected to receive no interventions due to an indolent clinical course such as MDS-RA (n=13). With a median follow-up of 1.9 years (range, 0.1–10.5) after the diagnosis of t-MDS/t-AL, the 3-year OS for all patients was 55%. Twenty-seven patients (median age, 48 years: range, 3–63) underwent allogeneic HCT from related (n=12) or unrelated (n=15) donors after myeloablative (n=18) or reduced-intensity (n=9) conditioning regimens. The sources of stem cells were BM in 15 patients, PBSC in 10, and CB in 2. At the time of HCT, 18 t-MDS/t-AL were in CR, 1 was in non-CR, and 8 had untreated t-MDS. Twenty patients (43%) did not undergo HCT due to various reasons, including age older than 65 years (n=11, treated before the introduction of nonmyeloablative transplant), indolent clinical course (n=4), progression of the primary disease (n=4) or t-AL (n=3), and patient refusal (n=2). The 3-year OS was significantly better in patients who received HCT than in those who did not (71% vs 31%; P=0.018; Figure). TRM after HCT was 15%. The 3-year OS was better in those who achieved CR after initial therapy for t-MDS/t-AL than in those who did not (74% vs 30%; P=0.002). A multivariate analysis revealed that HCT was associated with a significantly better OS, even after adjusting for age and other significant prognostic factors including achievement of CR in t-MDS/AL, cytogenetic risk group, and an interval between the diagnosis of primary disease and t-MDS/t-AL of longer than 3 years.
CONCLUSION: Although this study is contaminated by a selection bias, it still appears that HCT was an effective therapeutic option for patients with t-MDS/t-AL, especially when patients were in CR. These results support a prospective study to examine the value of upfront HCT, particularly for patients with an unfavorable cytogenetic risk.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal