Abstract
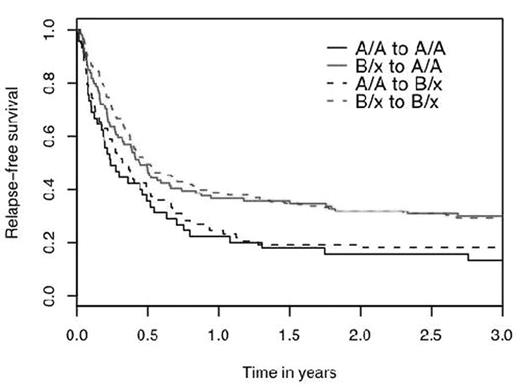
The importance of killer immunoglobulin-like receptors (KIR) in determining clinical outcome after hematopoietic cell transplantation (HCT) remains controversial. We analyzed 428 unrelated, T-cell replete transplants for acute myeloid leukemia (AML) facilitated by the National Marrow Donor Program between 1988 and 2003. Fifty seven KIR-ligand mismatched (thus HLA mismatched; KIR-Lmm/HLAmm) transplants were selected as cases. By matching on 15 clinical and demographic variables, KIR ligand matched, HLA mismatched (KIR-Lm/HLAmm; n = 162) and 10/10 HLA matched (HLAm; n = 209) comparison groups were selected. Using a validated single nucleotide polymorphism (SNP)-based MALDI-TOF assay, DNA samples were typed for 16 individual KIR genes which were used to estimate KIR haplotypes. About 1/3 of donors and recipients were A/A (lacking any activating KIR except 2DS4) and 2/3 possessed at least one B haplotype (B/X). As expected, 3 year survival was better in HLAm vs. HLAmm KIR-Lm or KIR-Lmm HCT (32%; p = .07 and 0.0004 respectively). However, survival was similar in both HLAmm groups (KIR-Lm 27% vs. KIR-Lmm 17%; p = .11). Importantly, transplants from donors with an activating B KIR haplotype had significantly better survival. Using a Cox regression that stratifies the baseline hazard according to sets of patients matched on important clinical variables, transplants using B KIR haplotype donors had a 42% reduced risk of mortality [B/X (vs. A/A) KIR haplotype donors (RR .58, 95% CI .44–.78; p = .0002]. Similarly, for disease-free survival (DFS), the risk of relapse and/or death decreased 43% [B/X (vs. A/A) RR .57, 95% CI .43–.76; p = .0001]. No differences were seen in risks of acute GVHD. The significant improvements in overall survival and DFS conferred by donor B KIR haplotype were seen in both the HLAm and KIR-Lm/HLAmm groups, but not in the KIR-Lmm/HLAmm group. The recipient KIR haplotype had no effect on outcomes, and the benefit of donor B KIR haplotype was equal regardless of recipient KIR haplotype (figure). Individual KIR genes were also analyzed and in Cox regression only donor 2DL2 and 2DS2 were favorable. As these genes are in strong linkage disequilibrium, the effects were similar (donor 2DL2 RR of death .70, 95% CI .54–.91; p = .008 and 2DS2 RR .66, 95% CI .50–.86; p = .002). 2DS2 defines a B KIR haplotype, confounding interpretation of these single gene effects. In summary, data from this analysis of the effect of KIR genes in unrelated T-replete HCT for AML suggest that using B KIR haplotype donors improves survival and DFS. Therefore, KIR genotyping could be incorporated into unrelated donor selection algorithms to identify B haplotype donors for patients with AML.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal