Abstract
BACKGROUND: A conditioning regimen for HLA-identical allogeneic hematopoietic cell transplantation in relapsed, refractory, or otherwise high risk myeloid malignancies has been developed, called FLAMSA (
PATIENTS AND METHODS: We have employed the FLAMSA protocol in 90 patients between March 2004 and June 2007, of whom 69 (the ident group) had a fully HLA-matched related (8/8 loci) or unrelated (10/10 loci) donor and 21 (the nonident group) a partially HLA-mismatched donor (1 locus in sixteen patients, 2 loci in four and haplo-identical in one). Half were females and half males, with a median age of 54 years (range: 19 to 71 years). 39 had been diagnosed with de novo acute myeloid leukemia (AML), 39 with secondary AML, 11 with myelodysplasia and one with acute lymphoblastic leukemia. 12 were in first and 4 in subsequent complete remission, whereas 74 were untreated, refractory or in relapse. Both the ident and the nonident groups were comparable regarding gender, age, diagnoses, cytogenetic risk group, remission status at transplant, as well as cytomegalovirus and sex match with their respective donor.
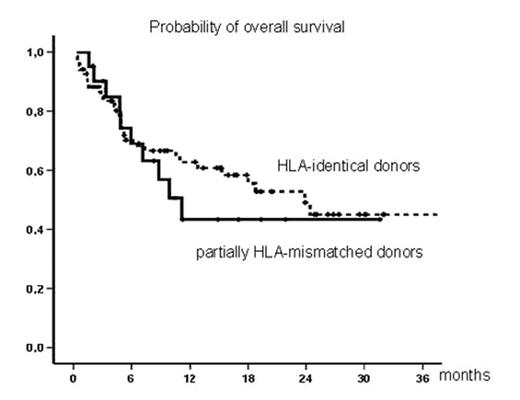
RESULTS: With 9.2 months (range: 0.3 to 38.2 months) median follow-up of all patients, 11/21 (52%) nonident patients are alive and 10/21 (48%) in complete remission, as compared to 39/69 (57%) ident patients (not significant). Probabilities of overall and disease-free survival at 2.5 years after allogeneic hematopoietic cell transplantation (Figure) are 43% and 35% for nonident and 45% and 41% for ident patients, respectively (p = 0.54 and p = 0.56; not significant). Treatment related mortality among nonident patients was 6/21 (29%) versus 12/69 (17%) in ident patients, whereas relapse related death occurred in 18/69 (26%) in the ident group with compared to 4/21 (19%) in the nonident group.
CONCLUSION: In our single-center, retrospective comparison with limited median follow-up, both fully HLA-identical and partially HLA-mismatched donors were suitable for the FLAMSA protocol. Confirmation of this finding in a prospective study is warranted.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal