Abstract
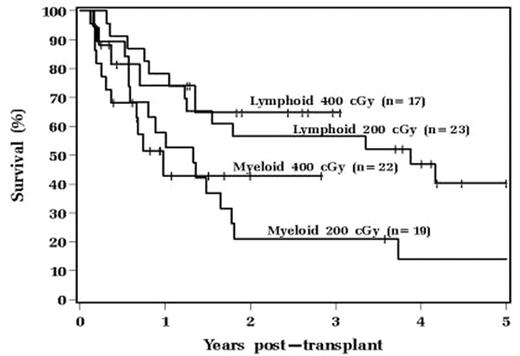
Fludarabine(FLU) and 200cGy TBI is commonly used for RIC AHSCT, but we observed 12% graft rejections and a 43% incidence of disease relapse when used at our institution. We hypothesized that this might be improved with dose escalation of TBI to 400cGy. From 12/03–4/07 40 pts with hematologic malignancies received RIC AHSCT using FLU 30 mg/m2/d on days -5, -4 and -3 and then TBI 200cGy on days -1 and 0. Our analysis compared outcomes with 42 historical control pts who received 200cGy TBI from 1/00–11/03. Matched sibling donors (MSD) were used for 32(76%) pts in the 200cGy group and 26 (65%) in the 400cGy group (p=0.27); other pts had 8/8 HLA matched unrelated donors (MUD). MSD pts received cyclosporine/mycophenolate and MUD pts received tacrolimus/mycophenolate. There were no differences in diagnostic categories between the 200cGy and 400cGy groups, which included 19(45%) and 22(56%) pts with myeloid (MY) diseases, respectively, (AML most common for both) while the remaining pts with lymphoid (LY) diseases had NHL most commonly. No other baseline characteristics differed between the groups. 200cGy pts received a higher median CD34+ cell dose (6.77 vs 4.93 × 106/kg, p<0.001), more often required 2nd transplants (5 vs 0; p=0.033) and donor lymphocyte infusions (5 vs 1; p=0.08) post RIC AHSCT. There were no differences in incidence or severity of acute/chronic GVHD, time to platelet and neutrophil engraftment, CMV, other infections or non-infectious toxicities. Although fewer 400cGy pts had graft rejection (2 vs 5), this did not reach statistical significance. Achievement of T cell complete donor chimerism (CDC) was similar between the 200cGy and 400cGy pts (85% vs 87%; p=0.61) as was the median time to achieve CDC (57 vs 40 days, respectively; p=0.80). Median times to achieve CDC for LY vs. MY pts were: 41 vs. 77 days (200cGy; p=0.26); and 30 vs. 61 days (400 cGy pts; p=0.29), respectively. Relapse rates for 200cGy and 400cGy groups were 43% vs. 30%; MY pts 42% vs 27% and LY pts 44% vs 29%, respectively. 12(29%) of the 200cGy pts and 23(58%) of 400cGy pts are alive at median follow-ups of 52 vs 16 mos, respectively. There was a trend toward higher 100 day mortality in the 400cGy pts with 7(18%) deaths (3 disease relapse, 2 cardiac, 1 GVHD, 1 graft failure) vs 2(5%) in the 200cGy pts (2 GVHD) (p=0.06). At current follow-up there are no significant differences in overall(OS) and relapse-free survival(RFS) between the groups. However, in the 200cGy group LY pts’ OS was superior to MY pts (p=0.047, Figure) but this difference was no longer observed upon escalating to 400cGy. This may be due to more comparable RFS between MY and LY pts in the 400cGy pts (p=0.56) than in the 200cGy group (p=0.07). We conclude that 400cGy TBI with FLU for RIC AHSCT is well tolerated and further follow-up is needed to determine if outcomes are superior to those with 200cGy TBI. Future investigation of strategies to further intensify RIC may be appropriate, particularly for pts with MY disease.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal