Abstract
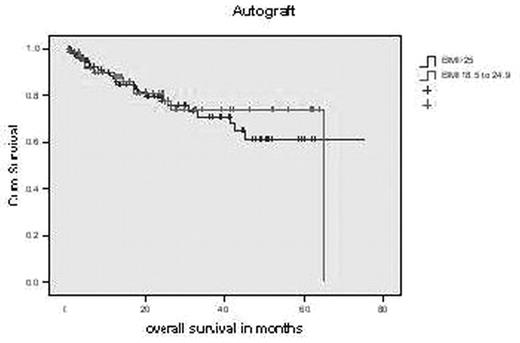
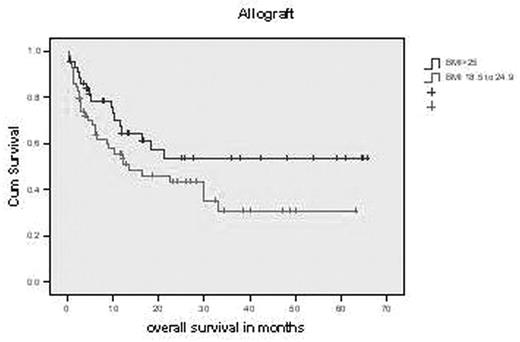
Bone marrow transplantation is frequently used as a consolidation therapy in patients with haematological malignancies to improve outcome. Obese individuals have larger absolute lean body and fat masses than non-obese individuals of the same age, gender and height, which might lead to altered pharmacokinetics of chemotherapeutic agents. Data on the impact of body mass on transplant outcome is conflicting. This study included 254 patients (M: 151; F: 103) with 283 transplant episodes (Autograft: 178, Allograft: 105). 81 patients had myeloma, 61 non Hodgkin’s lymphoma, 38 Hodgkin’s lymphoma, 34 acute myeloid leukaemia, 28 chronic lymphocytic leukaemia, 15 acute lymphoblastic leukaemia, 9 T cell non Hodgkin’s lymphoma, 6 each myelodysplasia and aplastic leukaemia and 1 each acute promyelocytic leukaemia and myelofibrosis. Statistical analysis was carried out using SPSS 13.0 for Windows. Overall survival (OS) and event free survival (EFS) were estimated by the Kaplan-Meier method. At transplantation 47% patients had normal & 52% high BMI. After a median follow-up of 14 month (range:0–75), mean OS in patients undergoing autograft with normal BMI was 52 months as compared to 54 with high BMI. Mean OS in patients undergoing allograft with normal BMI was 27 months as compared to 39 with high BMI (log rank test p value; autograft: 0.74 & allograft: 0.09). Odds Ratio for survival in autograft patients was 1.305 (95% CI: 0.611–2.786). For normal BMI patients OR for survival was 1.175(95% CI: 0.73–1.891), where as for high BMI patients 0.901 (95% CI: 0.678–1.197). Odds Ratio for survival in allograft patients was 0.512 (95% CI: 0.23–1.136). For normal BMI patients OR for survival was 0.751 (95% CI: 0.534–1.057), where as for high BMI patients 1.468 (95% CI: 0.921–2.341). Mean EFS in patients undergoing autograft with normal BMI was 42 months as compared to 50 with high BMI. Mean EFS in patients undergoing allograft with normal BMI was 26 months as compared to 48 with high BMI (log rank test p value; autograft: 0.4 & allograft: 0.3). This study shows that high BMI does not adversely impact on either OS or EFS in patients undergoing both autologous and allogeneic transplantation for haematological malignancies. On the contrary, the trend for OS appears to better in patients undergoing allograft with high BMI. We recommend patients with high BMI should not be excluded from having autologous transplantation. Studies with greater number of patients are needed to establish the potential beneficial impact of high BMI on survival in patients undergoing allogeneic transplantation.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal