Abstract
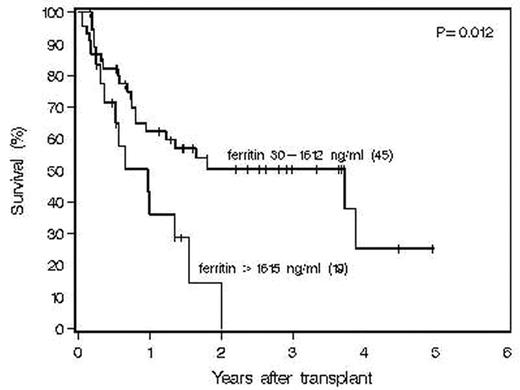
Iron overload is a well-established adverse prognostic factor for allogeneic hematopoietic stem-cell transplantation in thalassemia and appears to adversely affect prognosis with myeloablative transplantation for other diseases as well. In thalassemia, modification of the preparative regimen improves prognosis in patients who are at high risk due to iron overload. We analyzed a large group of patients who received a nonablative preparative regimen for allogeneic transplantation to determine whether the adverse impact of iron overload was circumvented by nonablative transplantation. Sixty-four consecutive patients undergoing nonablative allogeneic transplantation between 12/00 and 12/06 had pretransplant ferritin levels within 100 days preceding transplantation. Median age was 57 (range, 24–67) years; 24 patients were female. Median interval from diagnosis to transplant was 14.5 months (range, 2.4 to 151.6). Diseases included AML (n=16), NHL (15), MDS (10), myelofibrosis (6), CLL (6), CML (5), MM (3), Hodgkin (2), and ALL (1). Six had undergone prior transplantation. Median ferritin was 961 ng/mL (range, 302–6251). All but two received Flu/TBI preparation. Thirty-nine were sibling and 25 unrelated donors. Recursive partitioning identified significantly better survival for patients with ferritin ≤ 1615 ng/mL (n=45) compared to those with ferritin >1615 ng/mL (n=19; P=.012) as shown:
Among age, gender, diagnosis, interval from diagnosis to transplant, extent of therapy prior to transplant, ferritin level, albumin, AST, alkaline phosphatase, bilirubin, LDH, risk group, donor source, degree of HLA match, donor to recipient gender, and CD34+ dose, only ferritin >1615ng/ml (P=.010, HR= 2.74), older age (P=.049, HR= 1.63), and prior transplantation (p=.002, HR=5.78) were adverse prognostic factors for survival in multivariable analysis. The poorer survival was related to both a higher incidence of treatment-related mortality and a higher rate of relapse mortality, neither of which reached statistical significance. The addition of albumin, a negative acute phase reactant, did not change the prognostic impact of ferritin.
Conclusion: Similar to patients who undergo myeloablative transplantation, survival of patients who undergo nonablative allogeneic transplantation is adversely affected by elevated ferritin. It is important to assess the influence of specific factors on comparative results of myeloablative and nonablative transplantation. These results should stimulate study of iron chelation prior to allogeneic transplantations.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal