Abstract
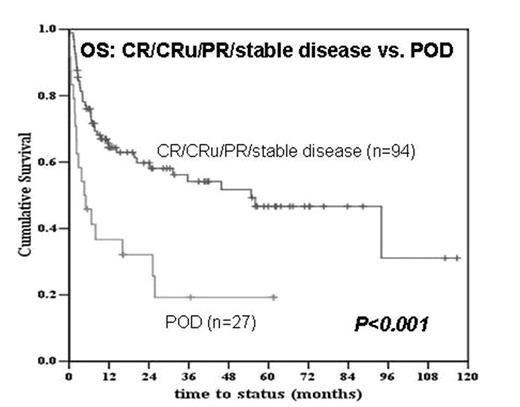
Chemosensitive disease is a requirement for successful autologous hematopoietic stem cell (HSC) transplant in patients with non-Hodgkin’s lymphoma (NHL) and Hodgkin lymphoma (HL). However, whether chemosensitivity is required for successful allograft is not well established. Therefore, we analyzed the survival of allograft recipients transplanted at MSKCC between 1995–2007 for the treatment of relapsed or refractory NHL and HL. Our hypothesis was that chemosensitive disease to pre-transplant salvage chemotherapy, as measured by functional and/or CT imaging, would be associated with improved survival post-allograft. One-hundred and twenty-one patients had pre-transplant imaging; 39 with aggressive NHL, 51 with indolent NHL, and 31 with HL by WHO classification. Following salvage chemotherapy, pre-allotransplant imaging revealed: 1) complete resolution of FDG/gallium-avid disease and/or decrease in lymphadenopathy to <1.5 cm (CR/CRu) (n=51); 2) partial remission (PR) or stable disease (n=46); or 3) progression of disease (POD) (n=24). The median age was 41 years (range 18–67) with 47 (39%) receiving ablative and 74 (61%) receiving less intensive conditioning. Forty-one (34%) had received prior autologous transplants. Patients were transplanted with HSC from either sibling donors (n=69), unrelated volunteer donors (n=40), or with cord blood (n=12). With a median follow-up of survivors of 26 months (range 2–117), the overall survival at 4 years post-transplant is 45%. While there was no difference in the survival of patients with CR/CRu and PR/stable disease (p=0.54), there was significantly worse survival for those patients with POD to pre-transplant salvage chemotherapy (p<0.001). However, 5/10 patients transplanted with progressive indolent NHL have survived in comparison to only 1/14 patients transplanted with POD of either aggressive NHL or HL. Notably, 11/18 (61%) deaths in the POD group were due to post-allograft relapse or disease progression. There was also a strong trend toward inferior survival for patients with prior autologous transplant (p=0.06). However, there was no significant difference in survival between patients aged < or ≥ 40 years, and recipients of ablative or less intensive conditioning.
In summary, determination of disease response by pre-transplant functional and/or CT imaging is a critical determinant of post allograft survival. Patients with CR/CRu or PR/stable disease fare equally well post-allograft. However, those with aggressive NHL or HL that is progressive pre-transplant do not benefit from allograft primarily due to death from post-transplant relapse/disease progression, and new strategies will be required to improve outcome in these patients. In contrast, patients with progressive indolent NHL may still benefit from allogeneic transplantation likely due to a more robust graft-versus-malignancy effect in this population.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal