Abstract
Recently, it has been suggested that concordant but not discordant BM involvement is a negative predictor of outcome in DLBCL patients treated with CHOP (Chung et al, Blood 2007). The significance of BM involvement in pts treated in the current era of therapy including rituximab has not been fully examined. We evaluated the prognostic impact of BM involvement in DLBCL patients treated with the current standard of care, R-CHOP.
Patients: We identified 282 patients with biopsy proven de novo DLBCL treated in British Columbia (BC) with an R-CHOP regimen between 01/01/2001 and 01/01/2005 with complete clinical information and staging bone marrows available for review. Cases were identified using the Lymphoid Cancer Database of the BC Cancer Agency. Median follow-up is 44 mos (range 1–77).
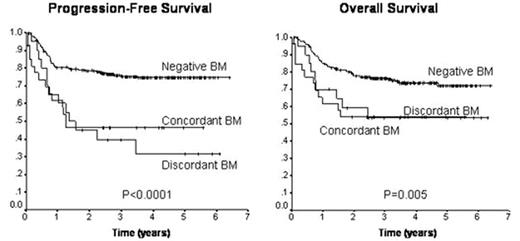
Results: 234/282 (83%) had a negative staging BM, 27 pts (10%) had a positive BM with concordant histology (Con-BM) and 21 (7%) had a positive BM with discordant histology (Dis-BM) with predominantly small B-cells present. Clinical characteristics for the entire cohort were as follows: median age 64 y (range 18–88); 66% male; 65% stage III/IV; 39% PS>1; 51% elevated LDH; 31% >1 extranodal site. IPI risk factors: 10% 0; 42% 1–2; 48% 3–5. In addition to higher stage and greater extranodal involvement, pts with a positive BM were more likely to have a higher LDH and a poorer PS than pts with a negative BM. Compared to pts with Con-BM, pts with Dis-BM were more likely to be elderly, but otherwise exhibited a similar distribution of clinical prognostic factors. The Kaplan-Meier 4-year PFS was significantly worse for pts with both Dis-BM (32%) and Con-BM (46%) involvement compared to pts with a negative BM (75%) (p<0.0001) (see Figure). Similarly, 4-year overall survival was significantly worse for pts with Dis-BM and Con-BM involvement (53% and 54%) compared to pts with a negative BM (74%) (p=0.005). All patients with Dis-BM involvement who developed progressive or relapsed disease were believed to have progression of their aggressive lymphoma based on clinical behavior or biopsy proof. In a multivariate analysis controlling for the IPI, BM involvement (Dis-BM and Con-BM) remained an independent predictor of PFS (p=0.03).
Conclusions: In DLBCL pts treated with R-CHOP, both discordant and concordant BM involvement predict for a poorer outcome independent of the IPI. It is possible that pts with DLBCL and discordant BM involvement represent a subset of pts with transformed disease which is inherently less treatment-sensitive.
Author notes
Disclosure:Employment: Both Wayne Saville and Dan Matso work for Biogen Idec. BiogenIdec provided funds to help support the lymphoma database. Consultancy: Roche, Genentech, Lilly, Johnson & Johnson, Biogen Idec. Research Funding: Roche Canada, Biogen Idec, Amgen, Bayer Healthcare, Genitope, Eli Lilly, Merck. Honoraria Information: Roche, Genentech, Lilly, Johnson & Johnson.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal