Abstract
Aim. The optimal management of IST in renal transplant patients with PTLD is uncertain. As chemotherapy regimens used for PTLD are in themselves immunosuppressive, IST may not be required during this phase of treatment. Subsequent long-term reduction in IST is important to prevent relapse. We examined whether a protocol (instituted in 1994) of ceasing IST during chemotherapy for PTLD and recommencing IST at reduced doses after chemotherapy (calcineurin inhibitor at 50%, prednisolone <6mg daily and no third agent) was associated with deleterious effects on renal graft function.
Methods. We performed a retrospective audit of adult renal transplant patients with PTLD requiring chemotherapy who were managed according to this protocol. Outcomes were compared (matched 1 case to 2 controls) to renal transplant patients without PTLD matched for age, gender, diabetes, graft type (cadaveric or live donor) and year of transplant. Matching was performed blinded to outcome.
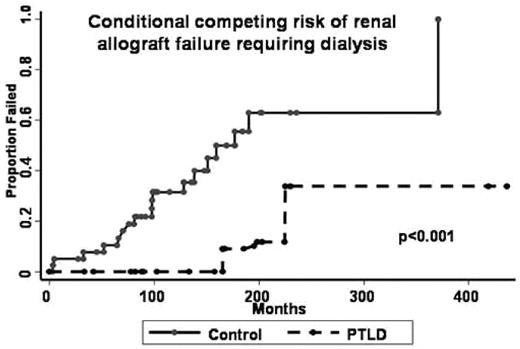
Results. 20 cases were identified: median age at PTLD diagnosis 39yrs; 85% male; 17 late onset PTLD; median time to onset of PTLD post-transplant 110 months (range, 5–276). 18 patients received prior triple combination IST (cyclosporine/tacrolimus plus azathioprine/mycophenolate mofetil plus prednisone). All patients received anthracycline-based chemotherapy with additional therapies of rituximab in 6 and radiation therapy in 4. 85% attained complete remission. 4 patients have relapsed. The 5yr OS was 75% with a median follow-up of 67 months from PTLD diagnosis. 6 cases (30%) had died (5 due to PTLD, 1 unknown) compared to 1 control (2.5%). Of the surviving 14 cases, 2 patients had failed renal allografts at 14 and 19yrs post-transplant and recommenced haemodialysis compared to 18 controls; neither case was retransplanted compared to 8 controls. 2 cases had >25% increment in serum creatinine but not requiring dialysis (assumed secondary to chronic allograft nephropathy) compared to 4 controls. 10 cases had normal functional allografts with no significant decrement in renal function. The cumulative rate of renal allograft failure requiring change of treatment to dialysis at 22yrs post-transplant was 34% vs 63% for cases and controls, respectively (p<0.05).
Conclusions. IST can be safely ceased during chemotherapy for PTLD in renal transplant patients and recommenced at reduced doses after chemotherapy, without deleterious effects on renal graft function.
Author notes
Disclosure: No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal