Abstract
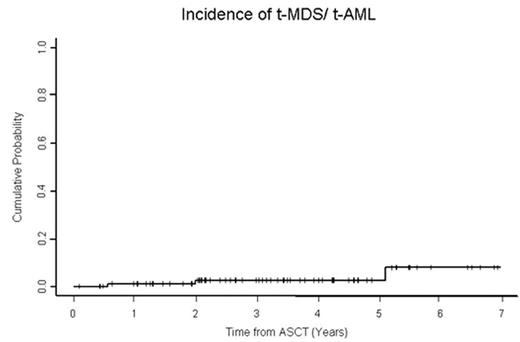
The reported incidence of t-MDS/t-AML following traditional ASCT for lymphoma ranges between 0–12%. Previously identified risk factors include older age, prior alkylator therapy and use of radiation either prior to ASCT or as part of the preparative regimen. It is unclear whether novel conditioning regimens for ASCT that utilize targeted RIT with the potential to deliver higher radiation doses to the marrow are associated with a higher risk of t-MDS/t-AML. We identified a case-series of 83 pts who underwent RIT based ASCT between 06/00 and 01/06 to evaluate the incidence of t-MDS/t-AML; Forty-one pts received standard dose 90Y ibritumomab tiuxetan (0.4mci/kg: median dose 32.9 mci (range 20–40)) in combination with high dose BEAM (BCNU 450mg/m2, etoposide 800mg/m2, cytarabine 800mg/m2, melphalan 140mg/m2) and 42 pts received high dose 90Y based on dosimetry (median 70.8 mci range 36–105) in combination with etoposide 60mg/kg plus cyclophosphamide 100mg/kg. Pts were followed prospectively post ASCT with serial bone marrow biopsies approximately annually. The median age at ASCT was 54 years (range 19–78). Disease histology included diffuse large cell n=40, follicular NHL n=17, mantle cell n=21, transformed n=4, SLL n=1. Disease status at ASCT was 1st CR n=17, 1stPR n=14, induction failure n=14, 1st relapse or greater n=38. With a median follow-up of 39 months (range, 1.4–83), three patients (3.61%) have developed t-MDS/t-AML. The three pts also had associated complex chromosomal abnormalities including de1(13q), del(5q), del (20q). The median time to t-MDS/t-AML was 2.63 years (range, 1.51 – 8.41) post NHL diagnosis and 1.99 years (range, 0.56 – 5.10) post ASCT. The cumulative incidences of t-MDS/t-AML at 1 and 2 years were 1.20% (95%CI, 0.17– 8.1%) and 2.60% (95%CI 0.64–9.9%). None of the potential risk factors including age(>50 at ASCT) (p=0.33), prior radiotherapy (p=0.99), number of prior regimens (p=0.5) and 90Y dose (p=0.99) were statistically significant by univariate analysis. As 82/83 pts had received prior alkylator therapy this was not analyzed as a separate risk factor. Two year overall survival for the entire cohort is 90% (95%CI 83–95). Although the follow up is relatively short, the incidence of t-MDS/t-AML is consistent with our previous institutional experience in ASCT patients who received non-RIT based conditioning (Krishnan et al. Blood 2000) and with the 2.5% incidence of t-MDS/t-AML observed in pts receiving 90Y in registration and compassionate use trials (Czuczman et al JCO 2007 in press). In conclusion RIT based conditioning does not appear to confer an increased risk of t-MDS/t-AML above what has been previously reported with traditional ASCT preparative regimens.
Incidence of t-MDS/t-AML
Author notes
Disclosure:Employment: Dr Molina is currently employed by Cougar Biotechnology ,however there is no COI with the study being presented. Ownership Interests:; Dr Molina is an officer in the company Cougar Biotechnology. Dr Krishnan has stock in Celgene, Amgen. Research Funding: Drs Nademanee and Raubitschek and Krishnan received research funding from Biogen Idec. Membership Information: Dr Raubitschek is on the speakers bureau for Biogen Idec. Dr Krishnan is on the speakers bureau for Genetech, Celgene, Millenium. Dr Fung is on the speakers bureau for Genetech. Financial Information: Dr Molina was previously employed by Biogen Idec during the conduct of the study. Off Label Use: The use of high dose Zevalin and Zevalin as part of a transplant preparative regimen are off label applications.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal