Dendritic cells (DCs) determine whether antigen presentation leads to immune activation or to tolerance. Tolerance-inducing DCs (also called regulatory DCs) act partly by generating regulatory T lymphocytes (Tregs). The mechanism used by DCs to switch toward regulatory DCs during their differentiation is unclear. We show here that human DCs treated in vitro with glucocorticoids produce the glucocorticoid-induced leucine zipper (GILZ). Antigen presentation by GILZ-expressing DCs generates CD25highFOXP3+CTLA-4/CD152+ and interleukin-10–producing Tregs inhibiting the response of CD4+ and CD8+ T lymphocytes. This inhibition is specific to the antigen presented, and only proliferating CD4+ T lymphocytes express the Treg markers. Interleukin-10 is required for Treg induction by GILZ-expressing DCs. It is also needed for the suppressive function of Tregs. Antigen-presenting cells from patients treated with glucocorticoids generate interleukin-10–secreting Tregs ex vivo. These antigen-presenting cells produce GILZ, which is needed for Treg induction. Therefore, GILZ is critical for commitment of DCs to differentiate into regulatory DCs and to the generation of antigen-specific Tregs. This mechanism may contribute to the therapeutic effects of glucocorticoids.
Introduction
Regulatory T lymphocytes (Tregs) play a key role in controlling immune responses. Initially, 2 types of Tregs were identified. Natural (or constitutive) Tregs are generated in the thymus and they spontaneously express the transcription factor FOXP3 and high levels of CD25. Inducible (or adaptive) Tregs are generated by peripheral activation, particularly in the presence of IL-10 or TGFβ. However, the relationship between these 2 subpopulations has not been completely elucidated. Tregs inhibit immune responses by a combination of effects requiring direct contact with their targets and the production of inhibitory cytokines, including IL-10 and TGFβ. In addition to the coexpression of CD25hi and FOXP3 and the production of IL-10 and TGFβ, several markers potentially characteristic of Tregs have been identified, but none of them has been unequivocally associated with the suppressive function of Tregs or with their classification into natural or inducible Tregs.1,,–4
Antigen presentation by dendritic cells (DCs) leads to either immune stimulation or tolerance. The mechanisms underlying the decision of DCs to orientate the immune response toward one of these 2 opposite outcomes are not fully understood. Tolerance-inducing DCs are also called regulatory DCs. One method used by regulatory DCs to prevent immune activation is to trigger T-lymphocyte anergy or apoptosis during antigen presentation. This involves production of the enzyme indoleamine 2,3-dioxygenase (IDO) and of nitric oxide by DCs.5,6 The other method is to generate regulatory cells, including Tregs. Although IDO production by DCs may play a role in the induction of Tregs,7 additional mechanisms are presumably involved. The state of maturation and activation of DCs is critical to Treg development: DCs activated and maturing in response to inflammatory stimuli trigger immune responses, but immature or “semimature” DCs, in contrast, induce tolerance,8,,–11 and this is in part mediated by the generation of Tregs.12,,–15 Phenotypically mature DCs can also be tolerogenic, and certain environmental signals can induce maturation of DCs in a tolerogenic mode.10 IL-10, TGFβ, glucocorticoids (GCs), vasoactive intestinal peptide, vitamin D3, and antioxidative vitamins, used alone or in combination, orientate DC maturation to induce tolerance,16,,,,,,,–24 and Treg development has been demonstrated for several of these agents.18,19,22,24 The molecular mechanisms involved in this switch of DC maturation toward regulatory DCs are largely unknown. Several tolerogenic agents down-regulate the NF-kB and p38 MAPK transduction pathways in DCs, which contrasts with the potency of inflammatory agents to activate them.24,25 In addition, DCs from RelB-deficient mice induce immune tolerance and antigen-specific Tregs.26 This suggests that modulation of NF-kB and p38 MAPK function contributes to the decision of DCs to differentiate into regulatory DCs.
An intracellular factor called glucocorticoid-induced leucine zipper (GILZ) was identified in mice thymocytes treated with GCs.27 GILZ blocks the NF-kB, p38 MAPK, and AP-1 transduction signals in several types of cells.28,29 We showed that GCs and IL-10 stimulate the production of GILZ by monocytes/macrophages, thus preventing their activation.30 GCs, IL-10, and TGFβ also stimulate the production of GILZ by human DCs, which results in an alteration of DC maturation. GILZ prevents expression of CD80, CD86, and CD83 and production of inflammatory chemokines by DCs. In contrast, GILZ stimulates their expression of B7-H1/CD274 and ILT3/CD85k and their production of IL-10.31 Therefore, GILZ inhibits the expression by DCs of immune-stimulating molecules and simultaneously up-regulates that of tolerogenic molecules.
We here analyzed the functional properties of CD4+ T lymphocytes stimulated by GILZ-expressing DCs. We found that such CD4+ T lymphocytes displayed Treg properties. The inhibitory function of Tregs was evidenced only when the same antigen was used for their induction and for the evaluation of their regulatory properties. IL-10 production by the Tregs was essential for inhibition. Antigen-presenting cells circulating in humans treated with GCs produced more GILZ, and this property explains their ability to generate Tregs ex vivo. These findings are the first demonstration that production of GILZ is involved in the decision of DCs to differentiate into Treg-inducing regulatory DCs, and that GCs, which are major therapeutic agents, use this mechanism to inhibit immune responses.
Patients, materials, and methods
Cell purifications and DC generation
Cells were isolated from buffy coats from the blood of healthy donors (Etablissement Français du Sang, Rungis, France). Monocyte-derived DCs were generated as previously described.31 Negative selection CD4+ T lymphocyte kit was used for CD4+ T-cell purification (Dynal, Compiègne, France). Purified CD4+ T lymphocytes comprised more than 96% of CD3+CD4+ cells and less than 1% CD11c+ILT3+ cells. CD4+ T lymphocytes and peripheral blood mononuclear cells (PBMCs) were kept frozen at −80°C until used. Unless specified, 10−7 M DEX (Sigma, St Quentin Fallavier, France) was added overnight to induce GILZ production by DCs. Antigens used were either PPD (1 μg/mL; Statens Serum Institute, Copenhagen, Denmark) or cytomegalovirus (CMV) extracts (1/2000; Bio Whittaker, Emerailville, France). DCs were nucleofected with siC or siGILZ 8 hours before DEX addition, as previously described.31 The fraction of transfected cells, determined using fluorescent siRNA, was between 40% and 75%. In other experiments, gene transfer experiments used the control vector pcDNA3 (pCTRL) and the GILZ-encoding vector pGILZ, which were introduced into DCs by nucleofection, as previously described.31 The fraction of transfected cells, determined by cotransfection of a green fluorescence protein–encoding vector, was between 50% and 70%. The day after nucleofection, DCs were pulsed with PPD or CMV for 4 hours, washed, and cocultured with autologous CD4+ T lymphocytes.
Functional studies of Treg function
DCs (2.5 × 104) were cocultured for 7 days with 1.25 × 105 autologous CD4+ T lymphocytes in 200 μL RPMI + 10% human AB serum (ABCYS, Paris, France). At the end of the stimulation, cells were 95% ± 2% CD3+CD4+ cells and 2% ± .5% CD11c+ILT3+. CD4+ T lymphocytes were purified, then irradiated (16 Gy), and added with PPD or CMV to autologous105 PBMCs labeled with 2.5 μM CFSE (5-(6)-carboxyfluorescein diacetate succinimidyl ester) according to the manufacturer's instructions (Vybrant kit; Molecular Probes, Eugene, OR). CFSE dilution in CD4+ responders was determined 5 days later. The numbers of CD4+ T lymphocytes added to CFSE-labeled PBMC was 105 for experiments performed with DCs nucleofected with pCTRL or pGILZ, and between 1.2 × 104 and 105 in experiments with siRNAs. Irradiated CD4+ T lymphocytes did not proliferate in the coculture with PBMCs, and less than 2% of CD4+ responders proliferated in the absence of antigen addition.
Western blot and immunoprecipitation studies
Detection of GILZ by Western blotting and by sodium dodecyl sulfate–polyacrylamide gel electrophoresis (SDS-PAGE) was as described.32 The anti-GILZ Ab used was a polyclonal antibody obtained by immunizing rabbits with a GST-GILZ fusion protein.32 GILZ was immunoprecipitated with the same rabbit antihuman GILZ Ab overnight and then the immune complex was separated with protein G (Sigma). Western blot results were quantified using ScanAnalysis software (BioSoft, Cambridge, United Kingdom), and results were expressed as GILZ/β-actin ratio.
Antibodies, flow cytometry, and ELISA studies
The following mouse mAbs were used: anti–CD4+-PC5, anti–CD4+-PE, anti–CD8+-PC5, anti–CD8+-PE (Beckman Coulter, Villepinte, France), anti–CD3+-antigen presenting cells (APCs), anti–CD25+-APCs, anti–CD25+-PE, anti–CTLA-4-Cychrome (BNI3) (BD Pharmingen, Pont-De-Claix, France), anti–GITR-PE (110416), anti–IL-10 mAb (25209) (R&D Systems, Lille, France), anti-PD1 (MIH4), and rat antihuman FOXP3 mAbs (PCH101) (eBioscience, Montrouge, France). Anti–LAG-3 mAb (S017/LPC1) was a gift from F. Triebel (Faculté de Pharmacie, Châtenay-Malabry, France). Negative controls were irrelevant isotype-matched mAbs. For combined detection of membrane and intracellular antigens, cell surface staining was performed first. Then, intracellular staining (for IL-10, CTLA-4, or FOXP3) was performed as recommended by the manufacturer (eBioscience). The data presented are gated for viable cells using light scatter. At least 104 events were acquired by flow cytometry (FACSCalibur; Becton Dickinson, Rungis, France) and analyzed using Cell Quest software (Becton Dickinson). The anti–IL-10 blocking mAb and its control (10 μg/mL; R&D Systems) were used for in vitro neutralization studies. Production of cytokines and chemokines was assessed using enzyme-linked immunosorbent assay (ELISA) kits from Diaclone (Besançon, France) for IL-10 and TNFα and from R&D Systems for CCL5.
In vivo induction of tolerogenic APCs
Blood was collected immediately before and 48 hours after initiation of oral prednisone treatment (.5 mg/kg of body weight/day) from patients with acute cervicobrachial neuralgia (n = 1) or symptomatic sinusitis (n = 2). All subjects gave written informed consent in accordance with the Declaration of Helsinki and research was approved by the local ethics committee of Antoine Beclere Hospital in Clamart, France. APCs were obtained by negative magnetic selection (Dynal), as described.31 Cell composition of APCs was determined in 3 experiments. APCs consisted of 9.5% ± 2.3% CD14+ILT3+ cells and of 2.9% ± 1.7% CD11c+ILT3+ cells. APCs were nucleofected with siC or siGILZ and pulsed 18 hours later with PPD. CD4+ T lymphocytes and PBMCs were purified before treatment and kept frozen until used. Purified CD4+ T cells were 96% or more CD4+CD3+ cells.
APCs (2.5 × 104) were cocultured with 105 CD4+ T lymphocytes for 7 days. At the end of the coculture, less than .5% of the cells were CD11c+ILT3+. Cells were irradiated and added to 105 CFSE-labeled PBMCs stimulated with PPD, and proliferation of responders was measured 5 days later.
Statistical analyses
Results are expressed as means ± SEM. Unless specified, the nonparametric Mann Whitney U test was used to analyze results. The nonparametric Wilcoxon test was used to analyze 3 different experiments. A P < .05 was considered as significant.
Results
Stimulation of CD4+ T lymphocytes by dexamethasone-treated DCs increases the fraction of CD25hiFOXP3+ cells
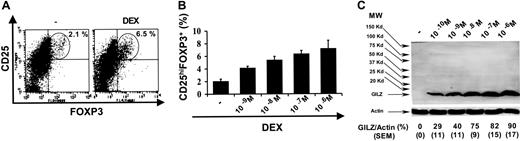
We investigated whether DCs treated with dexamethasone (DEX) stimulated the expression of Treg markers by CD4+ T lymphocytes. Human DCs treated or not treated with DEX during 18 hours were pulsed with purified protein derivative (PPD) and used to stimulate autologous CD4+ T lymphocytes. Seven days later, the expression of CD25 and FOXP3 by CD4+ T lymphocytes was analyzed. Compared with control DCs, DEX-treated DCs increased the fraction of CD4+ T lymphocytes coexpressing CD25hi and FOXP3, from 2.0% ± 0.2% for control DCs to 6.2% ± 0.3% for DEX-treated DCs (P < .05). A typical experiment is shown in Figure 1A. Dose-effect curves for DEX showed that the fraction of CD25hiFOXP3+ cells among CD4+ T lymphocytes was proportional to the concentration of DEX, with maximal induction of CD25hiFOXP3+ at 10−6 M DEX (Figure 1B).
Expression of CD25hi and FOXP3 by CD4+ T lymphocytes stimulated with DEX-treated DCs. (A-B) DCs were treated with DEX, pulsed with PPD, and used to stimulate CD4+ T lymphocytes. The fraction of CD25hiFOXP3+ cells among CD4+ T lymphocytes was then determined. Results representative of 5 experiments with DEX (10−7 M) are shown in panel A, and means ± SEM of 3 experiments with various concentrations of DEX are shown in panel B. (C) DCs were treated with various concentrations of DEX and production of GILZ was analyzed by Western blot. Quantification of actin was used as an internal control. MW indicates molecular weight markers. One representative of 3 experiments is shown on the top of the panel. The ratio between the intensities of GILZ and actin expressions in 3 experiments (mean ± SEM) is shown on the bottom of the panel.
Expression of CD25hi and FOXP3 by CD4+ T lymphocytes stimulated with DEX-treated DCs. (A-B) DCs were treated with DEX, pulsed with PPD, and used to stimulate CD4+ T lymphocytes. The fraction of CD25hiFOXP3+ cells among CD4+ T lymphocytes was then determined. Results representative of 5 experiments with DEX (10−7 M) are shown in panel A, and means ± SEM of 3 experiments with various concentrations of DEX are shown in panel B. (C) DCs were treated with various concentrations of DEX and production of GILZ was analyzed by Western blot. Quantification of actin was used as an internal control. MW indicates molecular weight markers. One representative of 3 experiments is shown on the top of the panel. The ratio between the intensities of GILZ and actin expressions in 3 experiments (mean ± SEM) is shown on the bottom of the panel.
GILZ production by DCs stimulates the expression of CD25hi, FOXP3, IL-10, and CTLA-4 by CD4+ T lymphocytes
We tested whether GILZ production by DEX-treated DCs contributed to their ability to increase the fraction of CD25hiFOXP3+ CD4+ T lymphocytes. GILZ production was assessed by Western blot analysis of DCs treated in vitro with various concentrations of DEX. No GILZ was produced in the absence of DEX. GILZ production was detected for DEX concentrations as low as 10−10 M, and the highest production was induced by 10−6 M (Figure 1C). Dose-effect curves of DEX were thus parallel for GILZ production by DCs and for their induction of CD25hiFOXP3+ on CD4+ T lymphocytes.
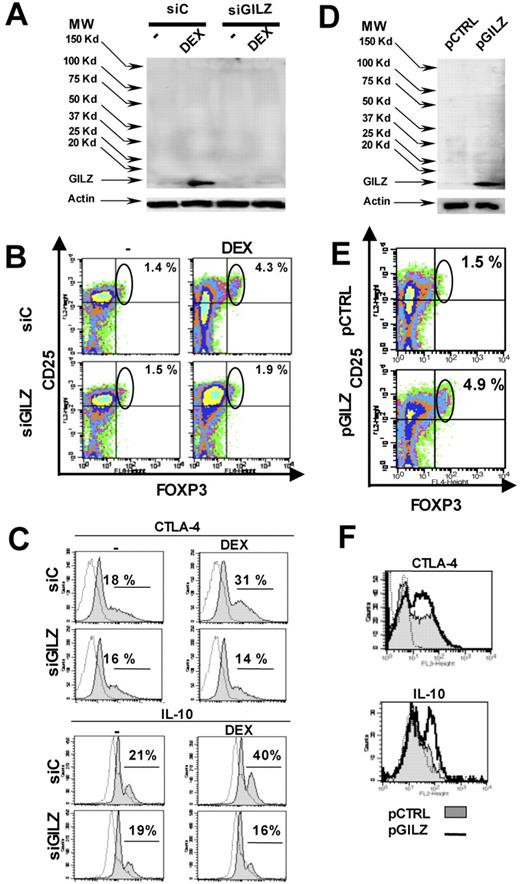
We then analyzed using small interfering RNA (siRNA) whether inhibition of GILZ production by DCs prevented the induction of CD25hiFOXP3+ CD4+ T lymphocytes. DCs were nucleofected with control (siC) or GILZ-specific (siGILZ) siRNA and were treated with DEX or control medium. Immunoprecipitation studies showed little or no GILZ in the absence of DEX addition, both in DCs nucleofected with siC (DCsiC) and in those nucleofected with siGILZ (DCsiGILZ). DEX increased the amount of GILZ in control DCs (DCsiC/DEX), but not in DCs nucleofected with siGILZ (DCsiGILZ/DEX) (Figure 2A). Therefore, GILZ siRNA efficiently inhibited GILZ expression by DCs. These different groups of DCs were pulsed with PPD and used to activate autologous CD4+ T lymphocytes: 4.6% (± 1.0%) of CD4+ T lymphocytes stimulated with DCsiC/DEX became CD25hiFOXP3+, compared with only 1.8% (± .8%) for DCsiC (P < .05, Wilcoxon test). This difference was not observed with DCs nucleofected with siGILZ: CD25hiFOXP3+ cells made up 1.9% (± .8%) of CD4+ T lymphocytes with DCsiGILZ and 2.0% (± .5%) with DCsiGILZ/DEX. A typical experiment is shown in Figure 2B. Therefore, production of GILZ by DEX-treated DCs was required to stimulate CD25 and FOXP3 expression by CD4+ T lymphocytes.
Induction of Tregs by GILZ-expressing DCs. (A-C) DCs were nucleofected with siC or siGILZ and treated or not treated with DEX (10−7 M). (D-F) DCs were nucleofected with the control vector (pCTRL, ▩) or the GILZ-encoding vector (pGILZ, −). (A,D) Production of GILZ was analyzed by immunoprecipitation. Quantification of actin was used as an internal control. (B-C,E-F) DCs were pulsed with PPD and used to stimulate autologous CD4+ T lymphocytes. Expression of Treg markers was determined by flow cytometry. Staining with a control mAb is shown as a dotted line in panels C and F. All results are representative of 3 to 5 experiments. MW indicates molecular weight markers.
Induction of Tregs by GILZ-expressing DCs. (A-C) DCs were nucleofected with siC or siGILZ and treated or not treated with DEX (10−7 M). (D-F) DCs were nucleofected with the control vector (pCTRL, ▩) or the GILZ-encoding vector (pGILZ, −). (A,D) Production of GILZ was analyzed by immunoprecipitation. Quantification of actin was used as an internal control. (B-C,E-F) DCs were pulsed with PPD and used to stimulate autologous CD4+ T lymphocytes. Expression of Treg markers was determined by flow cytometry. Staining with a control mAb is shown as a dotted line in panels C and F. All results are representative of 3 to 5 experiments. MW indicates molecular weight markers.
We next analyzed whether other Treg markers in addition to CD25hi and FOXP3 were induced in CD4+ T lymphocytes stimulated by GILZ-expressing DCs. Relative to DCsiC, DCsiC/DEX increased the expression of CTLA-4 and IL-10 by CD4+ T lymphocytes, but had no effect on GITR, PD1, and LAG-3 expression. No up-regulation of CTLA-4 and IL-10 expression was observed when DCsiGILZ/DEX were used to stimulate CD4+ T lymphocytes, implicating GILZ in this effect of DEX-treated DCs (Figure 2C and data not shown).
To determine whether GILZ production by DCs was sufficient to induce Treg markers on CD4+ T lymphocytes, DCs were nucleofected with a GILZ-encoding or a control vector. Presence of GILZ was detected in GILZ-transfected DCs but not in control DCs (Figure 2D). The DCs were pulsed with PPD and used to activate CD4+ T lymphocytes. The fraction of CD4+ T lymphocytes coexpressing CD25hi and FOXP3 was higher after activation with GILZ-transfected DCs (5.9% ± .6%) than with control DCs (2.6% ± 1.1%) (P < .05). A typical experiment is shown in Figure 2E. The direct role of GILZ in the induction of CTLA-4 and IL-10 expression was then investigated. We found that 22% (± 5%) of CD4+ T lymphocytes stimulated with control DCs and 38% (± 7%) of those stimulated with GILZ-transfected DCs expressed CTLA-4 (P < .05). The proportions for IL-10 expression were 16% (± 5%) and 45% (± 9%), respectively (P < .01). A typical experiment is shown in Figure 2F. GILZ-transfected DCs did not increase the expression of GITR, PD1, or LAG-3 by CD4+ T lymphocytes (data not shown). Altogether, these experiments showed that GILZ expression by DCs is sufficient to increase the expression of CD25hi, FOXP3, IL-10, and CTLA-4 by CD4+ T lymphocytes.
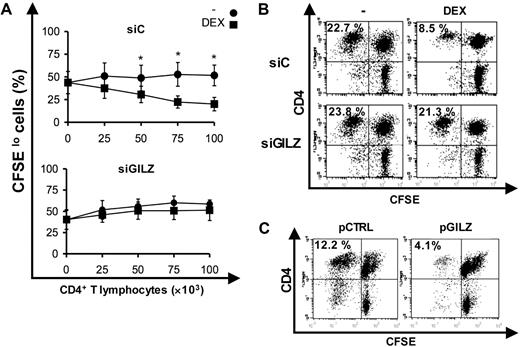
CD4+ T lymphocytes stimulated by GILZ-expressing DCs display regulatory functions
We next evaluated whether GILZ-expressing DCs generated CD4+ T lymphocytes with regulatory properties. To test suppressive functions, CD4+ T lymphocytes were purified at the end of the DC/CD4+ T lymphocyte coculture, irradiated, and added to CFSE-labeled autologous PBMCs stimulated with PPD. The proliferation of CFSE-labeled CD4+ T lymphocytes (CD4+ responders) was evaluated. The role of GILZ in the induction of Tregs was first tested by siRNA inhibition of GILZ expression in DEX-treated DCs. Compared with controls, CD4+ T lymphocytes stimulated with DCsiC/DEX inhibited the proliferation of CD4+ responders. Intensity of this inhibition was related to the number of CD4+ T lymphocytes added. In contrast, when DCsiGILZ/DEX were used to stimulate CD4+ T lymphocytes, CD4+ responder proliferation was not inhibited (Figure 3A-B). Thus, DEX-treated DCs generated CD4+ T lymphocytes with functional properties of Tregs, and production of GILZ by DCs was required for this effect.
Suppressive functions of CD4+ T lymphocytes stimulated with GILZ-expressing DCs. (A-B) Inhibition of GILZ expression and induction of Tregs. DCs, nucleofected with siC or siGILZ and treated or not treated with DEX (10−7 M), were pulsed with PPD and used to stimulate CD4+ T lymphocytes, which were then added in various numbers to CFSE-labeled PBMCs stimulated with PPD. Proliferation of CD4+ responders was assessed by flow cytometry. Means ± SEM of 7 experiments are shown in (A), and a representative experiment with 5 × 104 CD4+ T lymphocytes added to PBMCs is shown in (B). *P < .05. (C) Induction of Tregs by GILZ-transfected DCs. DCs were nucleofected with pCTRL or pGILZ, pulsed with PPD, and used to stimulate CD4+ T lymphocytes; the suppressive function of these lymphocytes was tested on the PPD-induced proliferation of CFSE-labeled CD4+ responders. Results shown are representative of 7 experiments. Percentages represent the fraction of CFSElo CD4+ T lymphocytes cells among CD3+CD4+ cells.
Suppressive functions of CD4+ T lymphocytes stimulated with GILZ-expressing DCs. (A-B) Inhibition of GILZ expression and induction of Tregs. DCs, nucleofected with siC or siGILZ and treated or not treated with DEX (10−7 M), were pulsed with PPD and used to stimulate CD4+ T lymphocytes, which were then added in various numbers to CFSE-labeled PBMCs stimulated with PPD. Proliferation of CD4+ responders was assessed by flow cytometry. Means ± SEM of 7 experiments are shown in (A), and a representative experiment with 5 × 104 CD4+ T lymphocytes added to PBMCs is shown in (B). *P < .05. (C) Induction of Tregs by GILZ-transfected DCs. DCs were nucleofected with pCTRL or pGILZ, pulsed with PPD, and used to stimulate CD4+ T lymphocytes; the suppressive function of these lymphocytes was tested on the PPD-induced proliferation of CFSE-labeled CD4+ responders. Results shown are representative of 7 experiments. Percentages represent the fraction of CFSElo CD4+ T lymphocytes cells among CD3+CD4+ cells.
We next evaluated the suppressive functions of CD4+ T lymphocytes stimulated by GILZ-transfected DCs: 29% (± 8%) and 14% (± 4%) of CD4+ responders proliferated when control DCs and GILZ-transfected DCs were used, respectively (P < .01). A typical experiment is shown in Figure 3C. Therefore, GILZ production by DCs was sufficient for the induction of Tregs.
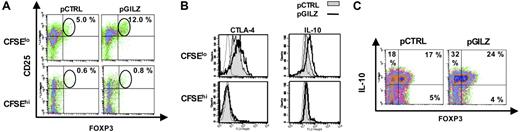
GILZ-transfected DCs stimulate the expression of Treg markers on antigen-specific CD4+ T lymphocytes
GILZ-expressing DCs increased the fraction of CD25hiFOXP3+ cells among CD4+ T lymphocytes. We investigated whether this effect was restricted to antigen-specific CD4+ T lymphocytes. Control and GILZ-transfected DCs pulsed with PPD were used to stimulate CD4+ T lymphocytes labeled with CFSE to identify antigen-specific T lymphocytes. The phenotype of CFSEhi and CFSElo CD4+ T lymphocytes (corresponding to nonproliferating and proliferating cells, respectively) was compared at the end of culture. Few CFSEhi CD4+ T lymphocytes coexpressed CD25hi and FOXP3, and this fraction did not substantially differ between cells stimulated with control or GILZ-transfected DCs (1.1% ± .6% and 1.2% ± .7%, respectively). In contrast, a significant fraction of CFSElo CD4+ T lymphocytes coexpressed CD25hi and FOXP3. There were more CD25hiFOXP3+ cells among CFSElo CD4+ T lymphocytes when GILZ-transfected DCs were used to activate T lymphocytes (14.2% ± 3.3%, compared with 6.8% ± 1.4% for controls, P < .05). A typical experiment is shown in Figure 4A.
GILZ-transfected DCs stimulate the expression of Treg markers by antigen-specific CD4+ T lymphocytes. Control and GILZ-transfected DCs were pulsed with PPD and used to stimulate CFSE-labeled CD4+ T lymphocytes. (A-B) Expression of Treg markers by CFSEhi and CFSElo CD4+ T lymphocytes was determined. A typical of 3 independent experiments is shown. Control mAb staining obtained with GILZ-transfected DCs is shown as a dotted line in panel B. (C) Expression of IL-10 and FOXP3 by CFSElo CD4+ cells was determined. A typical example of 2 independent experiments is shown.
GILZ-transfected DCs stimulate the expression of Treg markers by antigen-specific CD4+ T lymphocytes. Control and GILZ-transfected DCs were pulsed with PPD and used to stimulate CFSE-labeled CD4+ T lymphocytes. (A-B) Expression of Treg markers by CFSEhi and CFSElo CD4+ T lymphocytes was determined. A typical of 3 independent experiments is shown. Control mAb staining obtained with GILZ-transfected DCs is shown as a dotted line in panel B. (C) Expression of IL-10 and FOXP3 by CFSElo CD4+ cells was determined. A typical example of 2 independent experiments is shown.
As GILZ-transfected DCs increased the expression of CTLA-4 and IL-10 on CD4+ T lymphocytes, we tested whether this induction was also restricted to antigen-specific cells. Relative to controls, GILZ-transfected DCs increased CTLA-4 and IL-10 expression only in the CFSElo fraction of CD4+ T lymphocytes. No changes in GITR, PD1, and LAG-3 expression were observed (Figure 4B and data not shown). Therefore, GILZ-transfected DCs increased the expression of CD25hi, FOXP3, CTLA-4, and IL-10 only on antigen-specific CD4+ T lymphocytes.
Analysis of IL-10 and FOXP3 expression induced in T cells by GILZ-expressing DCs
The expression of several Treg markers by antigen-specific CD4+ T lymphocytes suggested that they were coexpressed by the same cells. We tested this hypothesis for the coexpression of FOXP3 and IL-10. In CFSElo CD4+ T lymphocytes stimulated with control DCs, approximately 75% of FOXP3+ cells expressed IL-10. However, a fraction of FOXP3− cells also expressed this cytokine, and IL-10+ FOXP3− cells were as abundant as IL-10+ FOXP3+ cells. GILZ-transfected DCs increased the fraction of CFSElo CD4+ T lymphocytes expressing IL-10. This applied to both FOXP3+ and FOXP3− cell subsets, but IL-10 induction was stronger for FOXP3− cells (Figure 4C). Therefore, GILZ-transfected DCs increased the expression of both FOXP3 and IL-10 on antigen-specific CD4+ T lymphocytes, but these 2 Treg markers were not necessarily found on the same cells.
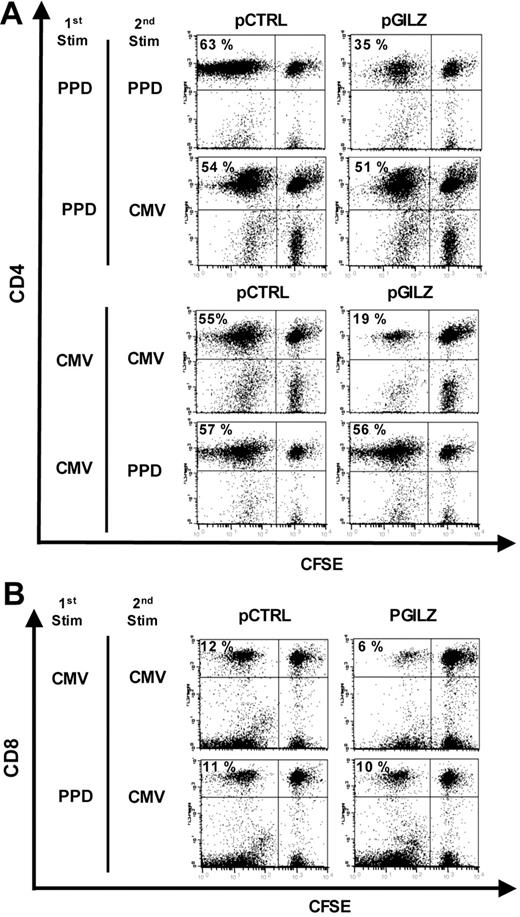
The suppressive function of Tregs induced by GILZ-transfected DCs is antigen-specific
The selective induction of Treg markers on antigen-specific CD4+ T lymphocytes suggested that the inhibitory effects of these cells could also be antigen specific. To test this hypothesis directly, control and GILZ-transfected DCs were pulsed with either PPD or CMV and used to stimulate autologous CD4+ T lymphocytes. The regulatory function of these cells was then tested on CD4+ responders stimulated with either PPD or CMV. Compared with controls, the Tregs induced by PPD-pulsed GILZ-transfected DCs inhibited the proliferation of CD4+ responders to PPD, but not to CMV (50% ± 3% inhibition [P < .05] and 8% ± 4% inhibition [P > .1], respectively). Conversely, the Tregs induced by CMV-pulsed GILZ-transfected DCs inhibited the proliferation of CD4+ responders to CMV, but not to PPD (62 ± 3% inhibition [P < .05] and 11% ± 6% inhibition [P > .1], respectively). A typical experiment is shown in Figure 5A.
Antigen specificity of the Tregs induced by GILZ-transfected DCs. (A-B) Control and GILZ-transfected DCs were pulsed with either PPD or CMV (first stimulation) and used to stimulate CD4+ T lymphocytes, which were then added to CFSE-labeled PBMCs stimulated with either PPD or CMV (second stimulation). Proliferation of CFSE-labeled CD4+ responders (A) and CD8+ responders (B) was assessed by flow cytometry. Results are representative of 4 experiments.
Antigen specificity of the Tregs induced by GILZ-transfected DCs. (A-B) Control and GILZ-transfected DCs were pulsed with either PPD or CMV (first stimulation) and used to stimulate CD4+ T lymphocytes, which were then added to CFSE-labeled PBMCs stimulated with either PPD or CMV (second stimulation). Proliferation of CFSE-labeled CD4+ responders (A) and CD8+ responders (B) was assessed by flow cytometry. Results are representative of 4 experiments.
We asked whether the CD4+ Tregs induced by GILZ-transfected DCs inhibited the proliferation of CD8+ T lymphocytes (CD8+ responders). Given the poor proliferative response of CD8+ T lymphocytes to PPD in most patients, proliferation of CD8+ responders stimulated with CMV was tested to address this issue. Compared with controls, Tregs induced by CMV-pulsed GILZ-transfected DCs inhibited the response of CD8+ responders to CMV (57% ± 5% inhibition, P < .05). Conversely, Tregs induced by PPD-pulsed GILZ-transfected DCs had little if any effect on the proliferation of CD8+ responders stimulated by CMV (12% ± 3% inhibition, P > .1). A typical experiment is shown in Figure 5B. Altogether, this indicated that the Tregs induced by GILZ-transfected DCs inhibited the response of both CD4+ and CD8+ responders, provided that the same antigen was used to generate Tregs and to test their inhibitory function.
Dual role of IL-10 in the induction of Tregs by GILZ-transfected DCs and in the suppressive function of Tregs
IL-10 is produced by GILZ-expressing DCs31 and favors the development of Tregs,9,33,–35 so we tested whether this cytokine was involved in the induction of Tregs by GILZ-transfected DCs. Control and GILZ-transfected DCs were pulsed with PPD and cocultured with CD4+ T lymphocytes. A neutralizing anti–IL-10 mAb or a control mAb was added to these cocultures. The suppressive function of CD4+ T lymphocytes on the proliferation of CD4+ responders was then determined. The anti–IL-10 mAb had no effect when control DCs were used to stimulate CD4+ T lymphocytes. In contrast, it abolished the induction of Tregs by GILZ-transfected DCs (Figure 6A). We then investigated whether IL-10 was involved in the suppressive function of the Tregs induced by GILZ-transfected DCs. The neutralizing anti–IL-10 mAb or the control mAb was added to cocultures of Tregs and CD4+ responders. In the presence of the anti–IL-10 mAb, the Tregs failed to inhibit the proliferation of CD4+ responders in response to PPD (Figure 6B). Therefore, IL-10 contributed in 2 different ways to the inhibition of lymphocyte responses by GILZ-transfected DCs: IL-10 was required for the induction of Tregs by GILZ-transfected DCs, and IL-10 produced by these Tregs contributed to their suppressive functions.
Role of IL-10 in the induction of Tregs and in their suppressive function. Control and GILZ-transfected DCs were pulsed with PPD and used to stimulate CD4+ T lymphocytes, which were then added to CFSE-labeled PBMCs stimulated with PPD. Proliferation of CD4+ responders was assessed by flow cytometry. (A) IL-10 is involved in the induction of Tregs. An anti–IL-10 mAb or its isotype control was added to the coculture of DCs and CD4+ T lymphocytes. (B) Production of IL-10 by Tregs is involved in their suppressive function. An anti–IL-10 mAb or its isotype control was added to the coculture of CD4+ T lymphocytes and responders. Results are representative of 3 experiments.
Role of IL-10 in the induction of Tregs and in their suppressive function. Control and GILZ-transfected DCs were pulsed with PPD and used to stimulate CD4+ T lymphocytes, which were then added to CFSE-labeled PBMCs stimulated with PPD. Proliferation of CD4+ responders was assessed by flow cytometry. (A) IL-10 is involved in the induction of Tregs. An anti–IL-10 mAb or its isotype control was added to the coculture of DCs and CD4+ T lymphocytes. (B) Production of IL-10 by Tregs is involved in their suppressive function. An anti–IL-10 mAb or its isotype control was added to the coculture of CD4+ T lymphocytes and responders. Results are representative of 3 experiments.
Antigen-presenting cells producing GILZ in vivo favor the development of Tregs
Administering oral GCs to patients increases GILZ expression by circulating APCs.31 To corroborate our in vitro findings in a more physiological settings, we investigated whether circulating APCs from patients treated with GCs induced Tregs ex vivo, and whether GILZ was involved in this phenomenon. We assessed the role of GILZ by nucleofecting APCs with siC or siGILZ. To confirm that this approach allowed to test GILZ modulation of APC functions, we evaluated the ex vivo production of cytokines and chemokines by LPS-stimulated APCs. APCs isolated from patients before GC treatment produced large amounts of CCL5, TNFα, and IL-10. The productions were similar between APCs nucleofected with siC (APCsiC) or with siGILZ (APCsiGILZ). APCs isolated after GC treatment and nucleofected with siC (APCsiC/GC) produced less CCL5 and TNFα than APCsiC but more IL-10. This difference was not detected when APCs from GC-treated patients were nucleofected with siGILZ (APCsiGILZ/GC): the amount of CCL5 and TNFα produced did not differ from pretreatment values, and less IL-10 was produced (Figure 7A). Therefore, ex vivo neutralization of GILZ by specific siRNA reversed changes of APC functions induced by GC treatment.
GILZ in APCs from GC-treated patients modulates the production of cytokines and chemokines and induces Tregs. APCs were collected before (■) and 48 hours after (▩) the initiation of GC treatment and they were nucleofected with siC or siGILZ. (A) APCs were stimulated with LPS and their production of CCL5, TNFα, and IL-10 was determined by ELISA (mean ± SEM). (B-D) APCs were pulsed with PPD and used to activate CD4+ T lymphocytes. (B) Expression of IL-10 by CFSElo CD4+ T lymphocytes was determined by flow cytometry. Control mAb staining obtained with APCs nucleofected with siC is shown as a dotted line. (C-D) CD4+ T lymphocytes were added in various numbers to CFSE-labeled PBMCs. Proliferation of CD4+ responders was assessed by flow cytometry. Means ± SEM from 3 experiments are shown in (A) and (C), and a representative experiment is shown in (B) and (D). CD4+ T lymphocytes (5 × 104) were added to PBMCs in panel D. *P < .05 using a Wilcoxon test.
GILZ in APCs from GC-treated patients modulates the production of cytokines and chemokines and induces Tregs. APCs were collected before (■) and 48 hours after (▩) the initiation of GC treatment and they were nucleofected with siC or siGILZ. (A) APCs were stimulated with LPS and their production of CCL5, TNFα, and IL-10 was determined by ELISA (mean ± SEM). (B-D) APCs were pulsed with PPD and used to activate CD4+ T lymphocytes. (B) Expression of IL-10 by CFSElo CD4+ T lymphocytes was determined by flow cytometry. Control mAb staining obtained with APCs nucleofected with siC is shown as a dotted line. (C-D) CD4+ T lymphocytes were added in various numbers to CFSE-labeled PBMCs. Proliferation of CD4+ responders was assessed by flow cytometry. Means ± SEM from 3 experiments are shown in (A) and (C), and a representative experiment is shown in (B) and (D). CD4+ T lymphocytes (5 × 104) were added to PBMCs in panel D. *P < .05 using a Wilcoxon test.
We then investigated the role of GC treatment and of GILZ on the induction of Tregs by circulating APCs. APCs collected before or after GC treatment were nucleofected with siC or siGILZ, pulsed with PPD, and used to stimulate CD4+ T lymphocytes collected before treatment. For Treg phenotype studies, these CD4+ T lymphocytes were labeled with CFSE and presence of IL-10 in CFSElo CD4+ T lymphocytes was tested. The fraction of CD4+ T lymphocytes expressing IL-10 was 16% (± 5%) with the use of APCsiC and 35% (± 6%) with APCsiC/GC (P < .05, Wilcoxon test). This increase was largely abolished when APCs were nucleofected with the GILZ siRNA. Only 21% (± 5%) CD4+ T lymphocytes expressed IL-10 when they were stimulated with APCsiGILZ/GC, and this was not different from results with APCsiGILZ (22% ± 4%). A typical experiment is shown in Figure 7B. Therefore, GILZ production was required for the induction of IL-10+ CD4+ T lymphocytes by APCs from GC-treated patients. To test whether CD4+ T lymphocytes stimulated with APCsiC/GC displayed suppressive functions, CD4+ T lymphocytes (not labeled with CFSE) were recovered at the end of the APC/CD4+ T lymphocyte coculture, irradiated, and added to CFSE-labeled PBMCs collected before treatment. CD4+ responders were stimulated with PPD and their proliferation was assessed. Compared with CD4+ T lymphocytes stimulated with APCsiC, CD4+ T lymphocytes stimulated with APCsiC/GC inhibited the proliferation of CD4+ responders. In contrast, CD4+ T lymphocytes stimulated with APCsiGILZ/GC had no effect on the proliferation of CD4+ responders (Figure 7C-D). Therefore, APCs isolated from GC-treated patients and used to activate CD4+ T lymphocytes generated cells with the phenotype and functional characteristics of Tregs, and the in vivo production of GILZ by these APCs was involved in Treg induction.
Discussion
We report a new mechanism orientating the differentiation of DCs, showing for the first time that GILZ contributes to the development of regulatory DCs and to the induction of antigen-specific, IL-10–secreting, CD25hiFOXP3+ Tregs. The decision of DCs to switch toward immune-stimulating or tolerance-inducing cells during their differentiation has major consequences, so this finding places GILZ at a critical crossroad in the regulation of the immune response.
GILZ expression conferred regulatory functions on human DCs. GILZ-expressing DCs, when presenting an antigen to CD4+ T lymphocytes, induced the expression of the Treg markers CD25hiFOXP3, CTLA-4, and IL-10 in those lymphocytes and this expression was restricted to proliferating cells. In addition, only CD4+ T lymphocytes activated by GILZ-expressing DCs displayed suppressive functions when tested on antigen-specific T-cell response assays.
GILZ-expressing DCs display several characteristics of tolerogenic DCs. They express lower levels of costimulatory molecules and produce lower amounts of inflammatory chemokines than conventional mature DCs.31 All these molecules are important for T-lymphocyte activation.10,36,37 It is however unlikely that the induction of Tregs by GILZ-expressing DCs resulted simply from a defective or partial activation of T lymphocytes. More likely, it resulted from an active process, in relation with the up-regulation of several tolerogenic molecules expressed by GILZ-expressing DCs. In particular, GILZ stimulates the expression of ILT3 and IL-10 by DCs,31 2 molecules favoring development of Tregs.9,33,–35,38,39 Although a contribution of ILT3 in our findings remains to be defined, IL-10 was essential for the generation of Tregs by GILZ-expressing DCs. Indeed, neutralization of IL-10 during cocultures of GILZ-expressing DCs and CD4+ T lymphocytes totally abolished the induction of Tregs.
The presence of Tregs among proliferating cells demonstrates their ability to expand on antigen challenge. IL-10 acts as a growth factor for Tregs in various models,9,33,–35 and this effect could explain why IL-10 was required for the emergence of Tregs in our conditions. Expression of GILZ by DCs did not influence viability of stimulated T lymphocytes (data not shown). Depletion of CD25+ cells from CD4+ T lymphocytes before their activation prevented the induction of Tregs by GILZ-expressing DCs (Figure S1, available on the Blood website; see the Supplemental Materials link at the top of the online article), and addition of CD25+ T lymphocytes to CD25-depleted cells restored Treg induction. GILZ-expressing DCs had no effect on IL-10 production by purified CD25+CD4+ T lymphocytes (Figure S2). All together, these results are consistent with an expansion of existing Tregs by GILZ-expressing DCs, rather than with an induction of suppressive functions in conventional T lymphocytes or in Tregs. This expansion involved only Tregs specific for the stimulating antigen, a property that may be of value for therapeutic applications.
IL-10 was also essential for the suppressive function of Tregs. Neutralization of IL-10 during the coculture of Tregs with responders totally reverted the inhibition of responder proliferation. We showed that the majority of FOXP3+ cells expressed IL-10, so this indicates that IL-10 is critical for the inhibitory function of FOXP3+ Tregs generated by GILZ-expressing DCs. The ability of CD25hiFOXP3+ natural Tregs to produce IL-10 in an antigen-specific manner has been demonstrated in various models in mice,40,,–43 and these cells expand vigorously in vivo after antigen challenge.40 Combined expression of FOXP3 and IL-10 by human Tregs has also been reported, with the intensity of FOXP3 expression by IL-10–secreting cells differing between experimental conditions.44,45 In these models, IL-10 was critical for the suppressive function of Tregs. We observed that GILZ-expressing DCs increased IL-10 production by CD4+ T lymphocytes regardless of their expression of FOXP3, showing that these Treg markers do not overlap exactly. It is therefore possible that IL-10–secreting FOXP3- CD4+ T lymphocytes also contributed to the suppressive function of Tregs in our experimental conditions.
The inhibitory effect of Tregs we describe was antigen specific: the Tregs induced by GILZ-expressing DCs presenting an antigen inhibited only responses to this specific antigen. This was observed whether the effect of Tregs was tested on CD4+ or CD8+ responders. Such antigen specificity suggests that during the suppression step, although inhibition was mediated by IL-10, TCR-mediated activation of Tregs by DCs presenting their cognate antigen was needed. This activation possibly increased the release of IL-10 by the Tregs, and the IL-10 then acted on APCs or directly on responders.
In addition to GCs, other agents promote the differentiation of regulatory DCs and favor induction of Tregs, raising the possibility that GILZ production by DCs could be a common mechanism shared by several tolerogenic agents. IL-10 and TGFβ, like DEX, stimulate GILZ production by DCs, and GILZ is involved in the DC phenotype changes these cytokines induce.30 In transgenic mice with forced production of IL-10 by DCs, these cells promote Treg differentiation in vivo.34 APCs from such mice produce unusually large amounts of GILZ.30 Both in humans and in mice, combined treatment with IL-10 and TGFβ generates regulatory DCs, which induce IL-10–secreting CD25+ Tregs.18,19 It remains to be determined whether production of GILZ by regulatory DCs is involved in these various models of tolerance induction.
Our findings for patients treated with GCs provide evidence that in vivo GILZ expression by DCs allows induction of Tregs. GC administration to patients increases the expression of GILZ by circulating APCs.31 We show that, when presenting an antigen to CD4+ T lymphocytes, these APCs generate Tregs, which produce IL-10 and suppressive effects. The contribution of GCs to the induction of Tregs has been shown previously. Some studies reported that GCs directly targeted CD4+ T lymphocytes.45,46 Two other studies in mice showed that GCs also target DCs: IL-10–secreting CD4+ T lymphocytes were induced by DCs treated in vitro with GCs and either vitamin D3 or LPS.47,48 The molecular mechanism involved in DCs was not defined. To our knowledge, the ability of GCs to promote the development of regulatory DCs in vivo has not been reported previously, either in mice or in humans. We also document the molecular mechanism of this effect, showing that it relies on GILZ production by DCs. Our findings thus reveal a new mechanism for the immunosuppressive action of GCs.
The demonstration of GILZ involvement in the development of regulatory DCs and in the generation of antigen-specific Tregs is of interest beyond just a better understanding of the therapeutic benefits of GCs. The molecular mechanism involved in the commitment of differentiating DCs toward immune-stimulating versus regulatory DCs has remained elusive, although down-regulation of NF-kB and p38 MAPK activities by tolerogenic agents appears to be involved. Our study was prompted by the ability of GILZ to inhibit both activities,28,29,30,49 joined to the observation that GILZ is induced in DCs by several tolerogenic agents.31 Our findings suggest various attractive possibilities for applications. For example, stimulation of GILZ production by DCs at the site of antigen presentation may be useful for the induction of antigen-specific tolerance by vaccination. Inclusion of the GILZ gene into recombinant vaccines and screening vaccine adjuvants for their ability to trigger GILZ production by DCs may help to design new tolerogenic vaccines for the treatment of allograft rejection, or autoimmune or allergic diseases.
The online version of this manuscript contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
This work was supported by the Agence Nationale de Recherche sur le SIDA (ANRS), the Association pour la Recherche sur le Cancer (ARC), the Fondation pour la Recherche Médicale, the European Union FP6 (INNOCHEM, grant number LSHB-CT-2005–518167, and the Université Paris-Sud (Bonus Qualité Recherche). H.H. holds fellowships from the ANRS and ARC.
We thank F. Triebel (Faculté de Pharmacie, Châtenay-Malabry, France) for providing the anti–LAG-3 mAb, C. Baillou for technical assistance, and M. Pallardy (Faculté de Pharmacie, Châtenay-Malabry, France) and I. Kryczek (Department of Surgery, Michigan University, Ann Arbor, MI) for helpful discussion.
Authorship
Contribution: H.H., W.Z., and D.E. designed the study. H.H., V.G., M.-C.M., M.V.P., and N.C. performed the research; F.M.L. provided important technical information and tools; H.H., R.K., and D.E. collected and analyzed the data; H.H. and D.E. wrote the paper; R.K., F.M.L., and W.Z. contributed to a critical reading of the paper; all authors read and approved the final paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Dominique Emilie, INSERM U764, 32 rue des Carnets F-92140 Clamart, France; e-mail: emilie@ipsc.u-psud.fr.



This feature is available to Subscribers Only
Sign In or Create an Account Close Modal