Abstract
The clinical course of polycythemia vera (PV) is marked by a high incidence of thrombotic complications; fibrotic and leukemic disease transformations are additional causes of morbidity and mortality. Major predictors of vascular events are increasing age and previous thrombosis; leukocytosis and high JAK2 V617F allele burden are currently being investigated for additional prognostic value in this regard. Myelosuppressive drugs can reduce the rate of thrombosis, but there is concern that their use raises the risk of transformation into acute leukemia. To tackle this dilemma, a risk-oriented management strategy is recommended. Low-risk patients should be treated with phlebotomy and low-dose aspirin. Cytotoxic therapy is indicated in high-risk patients, and the drug of choice is hydroxyurea because of its efficacy in preventing thrombosis and low leukemogenicity. Interferon-alpha should be reserved for selected categories of patients due to high cost and toxicity. The demonstration of JAK2 V617F mutation in the vast majority of PV patients opens the avenue for the development of promising new molecularly targeted drugs.
Introduction
Polycythemia vera (PV) is currently classified among the bcr/abl-negative, “classic” myeloproliferative disorders (MPDs), which also include essential thrombocythemia (ET) and primary myelofibrosis (PMF).1,2 Each of these MPDs represents a stem-cell–derived clonal myeloproliferation, with PV being characterized by a trilineage expansion of morphologically normal red cells, white cells, and platelets without significant bone marrow fibrosis.
Hematopoietic progenitors derived from patients with MPDs are hypersensitive to the stimulation of physiologic growth factors such as thrombopoietin or erythropoietin.3,4 This led investigators to search downstream receptor events, and pathophysiology of these diseases has advanced considerably with the recent discovery of an acquired mutation of JAK2 in a vast majority of PV patients and in almost half of those with ET and PMF.5–10 JAK2 is a member of the Janus kinase family of cytoplasmic tyrosine kinases that are associated with the intracellular domains of cytokine and growth factor receptors. The mutation, located within the negative regulatory pseudokinase, or Janus homology 2 (JH2) domain, replaces valine with phenylalanine in position 617 (V617F) of the JAK2 protein and causes cytokine-independent activation of several biochemical pathways implicated in erythropoietin receptor signaling.4–10
Besides molecular pathogenesis, the discovery of JAK2 V617F has had a major impact on the diagnostic approach to PV as well as the other MPDs.1 Traditionally, PV was diagnosed on the basis of a set of internationally recognized criteria established by the Polycythemia Vera Study Group (PVSG) and then the World Health Organization (WHO).11,12 However, the observation that more than 90% of patients with PV carry JAK2 V617F supports the recommendation that peripheral-blood mutation screening for the mutation be incorporated into the initial evaluation of all patients with suspected PV.1,2,4
Early studies in untreated PV patients found a high incidence of thrombotic events and a life expectancy of about 18 months after diagnosis.13 Cytoreductive treatments of blood hyperviscosity by phlebotomy or chemotherapy have dramatically reduced the number of thrombotic events, even though hematologic transformations toward PMF and acute leukemia still represent a major cause of death.14 Since there is a concern that myelosuppressive drugs given to control the proliferative phase of the disease might be implicated in the long-term complications, current treatment recommendations should be adapted on the expected risk for thrombosis of the patient.15
In this review, we address the following questions: (1) How do we stratify patients according to their thrombotic risk? (2) How do we treat low- and high-risk patients? (3) How do we manage special clinical situations, such as acute thrombohemorrhagic events, surgery, and pregnancy? For each of these problems, the relevant background is briefly discussed; approaches are recommended; and limitations of the available literature, along with needs for future research, are highlighted.
Incidence and type of thrombosis and hemorrhage
At initial presentation, the reported incidence of thrombosis and bleeding in PV patients varied from 12% to 39% and 1.7% to 20%, respectively.16 Factors that could have accounted for the relatively wide range of values include patient selection, definition of events, and accuracy in data reporting. The largest and most recent epidemiologic study (European Collaboration on Low-dose Aspirin [ECLAP]) included 1638 patients followed for a median of 2.8 years.14 A total of 164 deaths (10%) were recorded for an overall mortality rate of 3.7 per 100 persons per year. As compared with the general Italian population standardized for age and sex, the excess of mortality of PV patients was 2.1 times. Cardiovascular mortality accounted for 41% of all deaths (1.5 deaths per 100 persons per year), mainly due to large vessel arterial events, such as coronary heart disease and nonhemorrhagic stroke (Table 1). The cumulative rate of nonfatal thrombosis was 3.8 events per 100 persons per year, without difference between arterial and venous thrombosis. Major and fatal bleeding were rare, accounting for only 0.8 and 0.15 events per 100 persons per year. Thus, thrombosis still represents a major cause of morbidity and mortality in PV.
Main outcome events during follow-up (median 2.8 years) in 1638 patients with polycythemia vera
| Event . | No. of patients (%) . |
|---|---|
| All causes of mortality | 164 (10.0) |
| Fatal thrombosis | 67 (4.1) |
| Cardiac disease | 43 (2.6) |
| Ischemic stroke | 13 (0.8) |
| Pulmonary embolism | 6 (0.4) |
| Other vascular death | 5 (0.3) |
| Hemorrhagic death | 7 (0.4) |
| Fatal cancer | 54 (3.3) |
| Acute leukemia and myelofibrosis | 22 (1.3) |
| Other cancers | 32 (2.0) |
| Other cause of death | 36 (2.2) |
| Nonfatal thrombosis | 169 (10.3) |
| Arterial thrombosis | 87 (5.3) |
| Myocardial infarction | 14 (0.9) |
| Stroke | 23 (1.4) |
| Transient ischemic attack | 33 (2.0) |
| Peripheral arterial thrombosis | 20 (1.2) |
| Venous thrombosis | 88 (5.4) |
| Deep vein thrombosis | 38 (2.3) |
| Pulmonary embolism | 13 (0.8) |
| Superficial thrombophlebitis | 46 (2.8) |
| Event . | No. of patients (%) . |
|---|---|
| All causes of mortality | 164 (10.0) |
| Fatal thrombosis | 67 (4.1) |
| Cardiac disease | 43 (2.6) |
| Ischemic stroke | 13 (0.8) |
| Pulmonary embolism | 6 (0.4) |
| Other vascular death | 5 (0.3) |
| Hemorrhagic death | 7 (0.4) |
| Fatal cancer | 54 (3.3) |
| Acute leukemia and myelofibrosis | 22 (1.3) |
| Other cancers | 32 (2.0) |
| Other cause of death | 36 (2.2) |
| Nonfatal thrombosis | 169 (10.3) |
| Arterial thrombosis | 87 (5.3) |
| Myocardial infarction | 14 (0.9) |
| Stroke | 23 (1.4) |
| Transient ischemic attack | 33 (2.0) |
| Peripheral arterial thrombosis | 20 (1.2) |
| Venous thrombosis | 88 (5.4) |
| Deep vein thrombosis | 38 (2.3) |
| Pulmonary embolism | 13 (0.8) |
| Superficial thrombophlebitis | 46 (2.8) |
Patients with 2 or more events of different types can appear more than once in a column but only once in each row.
Particularly serious thrombotic events typically associated with PV are abdominal vein thrombosis (AVT), including Budd-Chiari syndrome and obstruction of the portal, mesenteric, and splenic systems. Overall, PV and other MPDs were reported to be the major cause of AVT, accounting for 25% to 65% of cases.17 Of importance, the diagnosis of MPD may be difficult in these disorders because blood cell counts and serum erythropoietin levels can still be within the normal limits or only slightly modified, and the presence of a splenomegaly is of little diagnostic value.17 Specialized tests, including bone marrow biopsy and endogenous erythroid colony formation, have been advocated,17 but a step forward in the diagnosis of an occult MPD in these patients has been done with the discovery of JAK2 V617F. Testing for the mutation was found positive in 40% to 58% % of patients with Budd-Chiari syndrome and 36% of those with portal vein thrombosis18,19 and is now recommended in all patients presenting with AVT.20
Rationale for risk stratification according to thrombotic risk
Age and previous thrombosis
Increasing age and a history of vascular events have consistently proven to be independent predictors of thrombosis in patients with PV.11,14 The first to report these risk factors were the PVSG investigators in a multivariate analysis of the entire cohort of 431 patients enrolled in the seminal 01 clinical trial (see also “Phlebotomy”). Phlebotomy treatment, rate of phlebotomy, history of prior thrombosis, and advanced age contributed significantly to the overall risk of thrombosis, whereas this was not found for other parameters such as sex and pretreatment hematologic indices (ie, hematocrit, white cell count, and platelet count).11 In the ECLAP study, the incidence of cardiovascular complications was higher in patients aged more than 65 years (5.0% patient-year, hazard ratio 2.0, 95% confidence interval [CI] 1.22-3.29; P < .006) or with a history of thrombosis (4.93% patient-year, hazard ratio 1.96, 95% CI 1.29-2.97; P = .002) than in younger subjects with no history of thrombosis (2.5% patient-year, reference category).14 At variance of the PVSG findings, performance of phlebotomy was not associated with an increased thrombotic risk (relative risk 0.89, 95% CI 0.67-1.18).
The predictive role of age and previous thrombosis for subsequent vascular events was also demonstrated in ET, providing further evidence for similar pathogenesis of thrombosis.21 Thus, age and history of thrombosis should be considered the current cornerstone for risk stratification and are an indication to begin cytoreductive drug therapy, regardless of other factors (Table 2)1,15,16
Risk stratification in polycythemia vera based on thrombotic risk
| Risk category . | Age older than 60 y or history of thrombosis . | Cardiovascular risk factors* . |
|---|---|---|
| Low | No | No |
| Intermediate | No | Yes |
| High | Yes | — |
| Risk category . | Age older than 60 y or history of thrombosis . | Cardiovascular risk factors* . |
|---|---|---|
| Low | No | No |
| Intermediate | No | Yes |
| High | Yes | — |
Extreme thrombocytosis (platelet count > 1500 × 109/L) is a risk factor for bleeding. Its role as a risk factor for thrombosis is uncertain. Increasing leukocyte count has been identified as a novel risk factor for thrombosis, but confirmation is required.
— indicates not applicable.
Hypertension, hypercholesterolemia, diabetes, smoking (see “Other risk factors”).
Platelet and leukocyte count
No study to date has demonstrated a significant correlation between platelet number or function and thrombosis.4,16 In the PVSG 01 clinical trial, platelet counts did not predict thrombosis, either measured at baseline or at the nearest times before the thrombotic event.11 Accordingly, a recent ad hoc analysis of the patients enrolled in the ECLAP study failed to show any association between platelet count and thrombotic events.22 Neither the currently proposed therapeutic target of 400 × 109/L nor any other of the platelet-count thresholds evaluated in this analysis predicted a higher risk of thrombosis. The concordant findings of these 2 major prospective studies in PV suggest that current treatment does not primarily aim at lowering the platelet count.
Leukocytosis was recently found to be an independent risk factor for thrombosis.23 PV patients with a white blood cell (WBC) count greater than 15 000 × 109/L, compared with those with a WBC count less than 10 000 × 109/L, had a significant 70% increase of the rate of vascular complications, mainly represented by myocardial infarction. Similar findings have recently been reported in patients with ET.24,25 In these disorders, in vivo leukocyte activation has been shown to occur and to be associated with signs of activation of both platelets and endothelial cells.26 Interestingly, platelet activation is increased in ET patients carrying the V617F JAK2 mutation, and in 1 study, a correlation between leukocytosis and the V617F JAK2 mutation was reported.25,27 Thus, leukocytes may play an important and hitherto underestimated role in the generation of the prethrombotic state of MPDs that is worthy of further exploration.
Other risk factors
Conventional risk factors for atherosclerosis, including hypertension, hyperlipidemia, diabetes, and smoking, have been assessed in PV with variable results, possibly reflecting the size of the studies and number of patients with the risk markers of interest included.14,16 In the absence of consistent data, it seems reasonable to assume that common cardiovascular risk factors are associated in PV with the same relative risk as those estimated in the general population. According to this assumption, recent guidelines recommend that all patients should be managed aggressively for their risk condition and should be requested to stop smoking.28 However, the use of cytotoxic drugs in otherwise low-risk patients carrying well-controlled cardiovascular risk factors is not generally indicated.16,28
Several studies have explored the contribution of inherited and acquired thrombophilic states to the occurrence of thrombotic events in PV with some conflicting results.16 To date, there is no convincing evidence that identification of a thrombophilic abnormality adds to the management of patients, so that routine thrombophilia screening is not currently recommended.28
Recently, the influence of the JAK2 V617F mutational load on the thrombotic risk has been evaluated in 96 patients with PV.29 A multivariate analysis including age, leukocytosis, hematocrit, platelet count, and treatment options indicated that the JAK2 V617F/JAK2 wild-type ratio behaved as an independent risk factor for major vascular events (P = .027). These data foresee the quantitation of JAK2 mutant allele as a promising approach for patient risk stratification in future studies.
Treatment of patients with a low risk for thrombosis
Phlebotomy
In the first randomized clinical trial (RCT) by the PVSG (01 study),11 431 patients were randomized to 1 of the following treatments: (a) phlebotomy alone; (b) radiophosphorus (32P) plus phlebotomy; or (c) chlorambucil plus phlebotomy. Patients treated with phlebotomy alone had a better median survival time (13.9 years) than those receiving 32P (11.8 years) or chlorambucil (8.9 years). Causes of death were different in the 3 groups. Phlebotomized patients showed an excess of mortality within the first 2 to 4 years, principally caused by thrombotic complications. Those in the 2 myelosuppression arms suffered higher rates of acute leukemia and other malignancies developing later during the follow-up. Hence, phlebotomy is recommended in all patients with PV and should represent the only cytoreductive treatment in patients at low risk for vascular complications.1,15,28
In this trial, the target hematocrit was set at 0.45 based on earlier evidence, suggesting a proportional increase of thrombotic events with high hematocrit.30 Those studies, however, were retrospective, included a small number of patients, and had methodological limits, such as the use of univariate analysis. In a recent multivariate analysis of a large prospective cohort of patients, a hematocrit in the evaluable range of 0.4 to 0.55 (40% to 55%) was associated neither with the occurrence of thrombotic events nor with mortality.22 Thus, an appropriate controlled study to establish the real hematocrit target in PV is needed. While waiting for such information, it seems prudent to maintain the recommended target at 0.45, with the caveat that no firm data exist to support this threshold or to differentiate the hematocrit target in men and women.
Phlebotomy should be started by withdrawing 250 to 500 cc of blood daily or every other day until a hematocrit between 0.4 and 0.45 (40% and 45%) is obtained. In the elderly or those with a cardiovascular disease, a smaller amount of blood (200 to 300 cc) should be withdrawn twice weekly. Once normalization of the hematocrit has been obtained, blood counts at regular intervals (every 4 to 8 weeks) will establish the frequency of future phlebotomies. Sufficient blood should be removed to maintain the hematocrit below 0.45 (45%). Supplemental iron therapy should not be given.
Aspirin
In a small-size RCT, the PVSG evaluated the role of aspirin in PV.31 A group of 166 patients was randomly assigned to the combination of high-dose aspirin (900 mg daily) plus phlebotomy and dypiridamole versus 32P. The trial was stopped because of an excess of major bleeding without the demonstration of efficacy in thrombosis prevention. This study had a significant impact on clinical practice: in a survey among American physicians it was reported that the use of aspirin was reserved to a minority of PV patients due to the concern of safety.32 In light of more recent knowledge of the dose requirements for selective antiplatelet therapy with aspirin,33 it appears that the PVSG study of platelet antiaggregating agents might have failed due to the use of excessive aspirin dosages. Low-dose aspirin regimens (40-100 mg daily) were much better tolerated and were associated with complete inhibition of platelet cyclooxygenase activity in pilot studies,34 providing the rationale for designing a formal RCT.
The ECLAP study randomized 518 PV patients to treatment with low-dose aspirin (100 mg daily) or placebo.35 Previous cardiovascular events were reported in only 10% of cases, so this trial included mainly an asymptomatic, low-risk population. Aspirin significantly lowered the risk of a primary combined end point including cardiovascular death, nonfatal myocardial infarction, nonfatal stroke, and major venous thromboembolism (relative risk 0.4 [95% CI 0.18-0.91]; P = .028). Total and cardiovascular mortality were also reduced by 46% and 59%, respectively. Major bleeding was only slightly increased by aspirin (relative risk 1.6, 95% CI 0.27-9.71). Given these results, low-dose aspirin (75-100 mg daily) is recommended in all PV patients without history of major bleeding or gastric intolerance.15,16,28
Treatment of patients with a high risk for thrombosis
Hydroxyurea
In the late 1970s, the search for a nonmutagenic myelosuppressive agent led the PVSG to investigate hydroxyurea (HU), an antimetabolite that prevents DNA synthesis by inhibiting the enzyme ribonucleoside reductase. At that time, it was assumed that this agent would not be leukemogenic or carcinogenic. In the last PVSG report,36 51 PV patients treated with HU were compared with 134 patients treated only with phlebotomy in the PVSG-01 protocol. There were no significant differences between the 2 groups, although the HU-treated patients showed a tendency to more acute leukemias (9.8% vs 3.7%), less myelofibrosis (7.8% vs 12.7%), and fewer total deaths (39.2% vs 55.2%).
Subsequently, HU was studied in 3 RCTs, 1 carried out in PV37 and 2 in ET.38,39 The only trial comparing HU with a randomized untreated control group was performed in 114 patients with ET and a high risk of thrombosis followed for a median of 27 months.38 A significant reduction of the rate of vascular events was observed in the HU arm (1.6% patient-year) compared with the controls (10.7% patient-year; P = .003). In a long-term follow-up study of these patients, an increase in secondary malignancies was observed only in those patients treated with HU who had previously been exposed to busulfan.40
In the second trial in ET, HU plus low-dose aspirin (100 mg daily) was compared with anagrelide plus low-dose aspirin in 809 high-risk patients analyzed with a median follow up of 39 months.39 Anagrelide is an inhibitor of megakaryocyte differentiation and proliferation with a selective platelet-lowering activity.41 Patients randomized to HU and aspirin were less likely to reach the composite primary end point of major thrombosis (arterial or venous), major hemorrhage, or death from a vascular cause (P = .03). Interestingly, the rate of thrombosis in the HU group in this trial (4% at 2 years) was similar to that in the HU group in the study reported in this paragraph.38
In PV, 292 patients below the age of 65 were randomized to treatment with HU or pipobroman and followed from 1980 until 1997.37 Pipobroman is an alkylating agent with a mechanism of action that also involves metabolic competition with pyrimidine bases. No significant differences between the 2 groups were observed in overall survival, rate of thrombotic complications, or incidence of secondary leukemia.
In these randomized studies, HU was demonstrated to be very effective in preventing thrombosis and thus should be considered the drug of choice in high-risk patients. Notably, the antithrombotic effect of HU may recognize additional mechanisms of action besides panmyelosuppression, including qualitative changes in leukocytes, decreased expression of endothelial adhesion molecules, and enhanced nitric oxide generation, as observed in patients with sickle-cell anemia.42,43
The starting dose of HU is 15 to 20 mg/kg/day until response is obtained (hematocrit < 0.45 [45%]). Thereafter, a maintenance dose should be administered to keep hematocrit at response levels without reducing WBC count values below 3000 × 109/L. Supplemental phlebotomy should be performed if needed. Complete hemogram should be recorded every 2 weeks during the first 2 months, then every month, and, in steady-state in responding patients, every 3 months.
Hematopoietic impairment, leading to neutropenia and macrocytic anemia, is the main toxic effect of HU. Other less-frequent side effects include oral and leg ulcers and skin lesions.44 The leukemogenic potential of this drug is still a matter of concern. Some retrospective and prospective studies found that a proportion of ET patients treated with HU developed acute leukemia, particularly those carrying cytogenetic abnormalities or those previously treated with other cytotoxic agents.36,37,40,45–47 In most series, however, this drug was rarely associated with secondary malignancies when used alone.40,46–48 The largest prospective study evaluated the leukemogenic risk of the 1638 patients enrolled in the ECLAP cohort, with a median disease duration of 6.3 years.49 HU alone did not enhance the risk of leukemia in comparison with patients treated with phlebotomy only (hazard ratio 0.86, 95% CI 0.26-2.88; P = .8). During the same period, the risk was significantly increased by exposure to radiophosphorus, busulfan, or pipobroman (hazard ratio 5.46, 95% CI 1.84-16.25; P = .002). The use of HU in patients already treated with alkylating agents or radiophosphorus also enhanced the leukemic risk (hazard ratio 7.58, 95% CI 1.85-31; P = .005). Translated evidence of the long-term safety of HU comes from the experience with sickle-cell anemia patients, including children, who did not develop an excess of leukemic transformation for up to 10 years after treatment.50
To date, the bulk of evidence does not support a clear leukemogenic risk for HU. However, there are no randomized studies powered to assess the relative risk of malignant transformation in MPD patients given this agent. Thus, it is wise to adopt a cautionary principle and to carefully consider the use of this agent in young subjects and in those previously treated with other myelosuppressive agents or those carrying cytogenetic abnormalities.
Interferon α (IFNα)
The use of IFNα in PV has been pioneered by Silver.51 IFNα suppresses the proliferation of hematopoietic progenitors, has a direct inhibiting effect on bone marrow fibroblast progenitor cells, and antagonizes the action of platelet-derived growth factor, transforming growth factor-β, and other cytokines that may be involved in the development of myelofibrosis.52
IFN is contraindicated in patients with thyroid and/or mental disorders; for this reason an accurate evaluation of thyroid function and inquiry of previous or present mental disorders in candidate patients are recommended. IFN should be administered at the dose of 3 million units (MU) daily until a response is reached (hematocrit < 0.45 [45%]); then, maintenance therapy has to be adjusted at the lowest weekly doses that control the hematocrit at response level. Complete hemogram must be recorded every week during the first month of therapy, every 2 weeks during the second month, then every month and, in steady-state in responding patients, every 3 to 4 months. Peg-IFN is given at a starting dose of 0.5 μg/kg once weekly. In patients who failed to achieve a response after 12 weeks, the dose is increased up to 1.0 μg/kg/week. Then, therapy has to be adjusted at the lowest dose that maintains the response and monitored as described for IFN.
Published reports concern small consecutive series of patients in whom hematologic response and side effects were evaluated. One review analyzed the cumulative experience with IFNα in 279 patients from 16 studies.53 Overall responses were 50% for reduction of hematocrit to less than 0.45% without concomitant phlebotomies, 77% for reduction in spleen size, and 75% for reduction of pruritus. In a recent review article, Silver54 updated his experience with the long-term use (median 13 years) of IFNα in 55 patients with PV. Complete responses, defined by phlebotomy free, hematocrit less than 0.45 (45%), and platelet number below 600 × 109/L, were reached in the great majority of cases after 1 to 2 years of treatment, and the maintenance dose could be decreased in half of the patients. Noteworthy is the absence of thrombohemorrhagic events during this long follow-up.
The main problem with IFNα therapy, apart from its costs and parental route of administration, is the incidence of side effects. Fever and flulike symptoms are experienced by most patients and usually require treatment with paracetamol. Signs of chronic IFNα toxicity, such as weakness, myalgia, weight and hair loss, severe depression, and gastrointestinal and cardiovascular symptoms, make it necessary to discontinue the drug in about one third of patients.53 Overall, the role of IFNα in PV therapy requires controlled clinical trials evaluating long-term clinical end points.
Recently, semisynthetic pegylated forms of interferon-α (peg-IFNα) have been used to treat MPDs, which in a limited number of studies have been shown to be superior to unmodified IFN as related to its adverse event profile and efficacy.55 In 1 study, the use of peg-IFNα-2a was able to decrease the percentage of mutated JAK2 allele in 24 of 27 treated PV patients from a mean of 49% to a mean of 27%.56 A more limited effect of other forms of nonpegylated or pegylated IFNα (peg-IFNα-2b) on JAK2 mutational status has been reported.57,58 Further studies are needed to establish whether the reduction of JAK2 V617F allele burden is clinically relevant and whether its monitoring during therapy is of any value.
Due to its high cost and toxicity, IFNα should be reserved to selected categories of patients such as pregnant women, very young subjects, or those with intolerance to HU or intractable pruritus.
JAK2 mutation as target of therapy
The description of the V617F point mutation in the JAK2 kinase of patients with PV has generated great interest in determining if patients would be sensitive to small molecular agents specific to the pseudokinase domain of JAK2 or to other tyrosine-kinase inhibitors.
Pilot clinical studies have explored whether imatinib may have a role in PV. Jones et al59 have reported responses in a small group of PV patients at doses up to 800 mg per day. Imatinib was effective in reducing phlebotomy requirements, lowering abnormal platelet counts, and reducing spleen size. The relation of imatinib treatment and JAK2 mutation was evaluated by Jones et al57 in 9 PV patients for whom pretreatment samples were available. They reported 2 cases who achieved complete hematologic remission and a 2- to 3-fold reduction in the percentage of V617F alleles. However, the clinical experience with this drug is still very limited and we do not recommend imatinib for the current treatment of patients with PV.
A series of more specific JAK2 V617F inhibitors with promising potency and pharmaceutical properties for utility in the therapy of PV have been recently synthesized.60–62 Preliminary data indicated that at least some of these small molecules inhibit cell growth that is dependent on constitutive JAK2/STAT signaling and preferentially suppress growth of progenitors carrying JAK-activating mutations. Thus, these drugs hold promise as molecularly targeted agents for the therapy of patients with PV.
Management of acute events
Bleeding
Major bleeding is rare in patients with PV. The main sites affected are skin, mucous membranes, and gastrointestinal tract. Intracranial bleeding occurs occasionally but can be severe and potentially fatal. Intra-articular, retroperitoneal, and deep intramuscular hematomas, like those seen in hemophilia, are distinctly unusual.16
Hemorrhagic symptoms are more frequent in patients with platelet counts in excess of 1500 × 109/L and this may be related to an acquired disease von Willebrand (AVWD).63 AVWD in MPD patients is characterized by the loss of large von Willebrand factor (VWF) multimers that results in a functional defect of the protein, with increasing platelet counts. Normalization of the platelet count was accompanied by restoration of a normal plasma VWF multimeric distribution and regression of the hemorrhagic tendency.63 Qualitative platelet abnormalities in PV have long been investigated but there is a disappointing lack of clinical correlation with hemostatic complications.16,64 These abnormalities have not been shown to have any relevant role in the management of bleeding.16,28,64 Serious hemorrhages may be triggered by simultaneous antithrombotic therapy with anticoagulants or antiplatelet agents. These drugs should be avoided in PV patients with previous hemorrhagic events, including symptomatic AVWD, or anatomical conditions with a high bleeding risk (eg, gastric ulcers or esophageal varices secondary to AVT and portal hypertension).
Treatment of major bleeding events in PV should start with withdrawal of any concomitant antithrombotic therapy and correction of thrombocytosis. This latter situation is usually treated with HU, particularly if associated with AVWD. Other potential measures include antifibrinolytic agents such as tranexamic acid (1 g every 6 to 8 hours), desmopressin (0.3 μg/kg/d), or VWF-containing therapeutic products.16,28,64 However, the reported clinical experience with these drugs in PV is very limited.
Thrombosis and secondary thromboprophylaxis
Acute vascular events should be managed according to the current guidelines.65 Patients with venous thromboembolism should be given low–molecular-weight heparin (LMWH) at therapeutic doses followed by warfarin, with the aim of keeping Prothrombin Time International Normalized Ratio (PT INR) in the conventional therapeutic range (2.0-3.0). Close clinical and laboratory monitoring has been recommended because of a potentially greater bleeding risk and unpredictable drug influences in MPD patients.16 However, it is still not clear whether to give warfarin for 3 to 6 months, according to standard practice, or to continue with long-term prophylaxis, considering that MPD is an important persistent risk factor for thrombotic recurrences. Life-long warfarin prophylaxis has been advocated for patients with AVT. 66,67
Symptomatic patients presenting with severe microvascular circulation disturbances, such as erythromelalgia, should immediately be treated with a loading dose of aspirin (300 to 500 mg per day) followed by a lower maintenance dose (100 mg per day).68 Low-dose aspirin therapy (100 mg per day) is also recommended for patients with a recent major arterial vascular event (ischemic stroke, transient ischemic attack, peripheral arterial occlusion, myocardial infarction, unstable angina) or for whom there is clinical and laboratory evidence of coronary artery disease, provided there is no contraindication to antiplatelet therapy.16,28
Appropriate cytoreduction with the goal to optimize the control of the blood cell counts is recommended in all patients with acute vascular events (Table 3)28 In a recent analysis of recurrent thrombosis in 470 patients with PV and ET, cytoreductive treatment halved the probability of both arterial and venous recurrences (hazard ratio 0.54, 95% CI 0.38-0.76).69
Recommendations for management of pregnancy in polycythemia vera
| Risk stratification: at least 1 of the following defines high-risk pregnancy |
| Previous major thrombotic or bleeding complication |
| Previous severe pregnancy complications* |
| Therapy |
| Low-risk pregnancy |
| Target hematocrit should be kept below 0.45 (45%) |
| Aspirin 100 mg/day |
| LMWH 4000 U/day for the first 6 weeks after delivery |
| High-risk pregnancy |
| As described for low risk, plus: |
| If previous major thrombosis or severe pregnancy complications, LMWH 4000 U/day throughout pregnancy (stop aspirin if bleeding complications). |
| If myelosuppression is required, consider IFN-α† |
| Risk stratification: at least 1 of the following defines high-risk pregnancy |
| Previous major thrombotic or bleeding complication |
| Previous severe pregnancy complications* |
| Therapy |
| Low-risk pregnancy |
| Target hematocrit should be kept below 0.45 (45%) |
| Aspirin 100 mg/day |
| LMWH 4000 U/day for the first 6 weeks after delivery |
| High-risk pregnancy |
| As described for low risk, plus: |
| If previous major thrombosis or severe pregnancy complications, LMWH 4000 U/day throughout pregnancy (stop aspirin if bleeding complications). |
| If myelosuppression is required, consider IFN-α† |
Severe pregnancy complications: at least 3 first-trimester losses or at least 1 second- or third-trimester loss; birth weight lower than the fifth centile of gestation; preeclampsia; intrauterine death; or stillbirth.
Disease-related prior reason for cytotoxic therapy or uncontrolled hematocrit or progressive myeloproliferation (leukocytosis, thrombocytosis, splenomegaly).
Pruritus
Intractable pruritus, typically aquagenic, can represent a disabling condition in some patients with PV. A number of small studies have tried to address this problem.28 Antihistamines, such as cyproheptadine 4 to 16 mg/d, may be of benefit. If unsuccessful, interferon-α therapy (3.0 × 106 units subcutaneously 3 times a week) was reported to be effective in the majority of patients.53 Other treatment options include paroxetine (20 mg/d70 ), a selective serotonin uptake inhibitor, and photochemotherapy using psoralen and ultraviolet A light.71
Special management issues
Pregnancy and women of childbearing age
PV is rare in women of childbearing age. The estimated incidence ranges from 0.04 per 100 000 in women aged 20 to 34 years to 0.25 per 100 000 in those aged 35 to 39 years.72 Thus, only limited evidence is available to give practical recommendations for management.72–74 The most updated study reported a series of 18 pregnancies in 8 women with PV and reviewed the literature for a total of 38 pregnancies in 18 patients.75 A better outcome of pregnancies was observed when these women were followed in a specialist myeloproliferative clinic and treated according to a formal predefined protocol. Patients should be stratified according to the risk of developing thrombosis or pregnancy complications, and preconception planning, including cessation of possible teratogenic medications, and precise control of hematocrit before pregnancy should be offered. The target hematocrit should be kept below 0.45 (45%) and all patients should receive low-dose aspirin throughout pregnancy and prophylactic LMWH for 6 weeks postpartum. In high-risk patients requiring myelosuppressive therapy, IFNα is considered the drug of choice. Treatment recommendations are summarized in Table 3.
Surgery
Patients with MPDs have an increased risk of morbidity and mortality when they require surgical procedures. In a recent survey on the outcome of 311 surgical interventions in 105 patients with PV and 150 with ET, 24 arterial or venous thrombosis–related deaths (7.7%), 23 major hemorrhage–related deaths (7.3%), and 5 surgery-related deaths (1.6%) were observed within 3 months from the procedure.76 The optimal management is uncertain because of the lack of controlled trials. The appropriate control of erythrocytosis and thrombocytosis with phlebotomy and/or myelosuppression has been recommended.16 Aspirin should be withheld for at least 1 week before elective surgery involving a high risk of bleeding or in which even minor bleeding could result in life-threatening complications, such as neurosurgery, or requiring heparin prophylaxis. The drug can be restarted 24 hours after stopping heparin. LMWH at a prophylactic dose (4000 U subcutaneously starting 12 hours before surgery) is probably indicated in all patients with MPD because of the high thrombotic risk, although there are no prospective studies in this setting. Finally, these patients must be followed carefully for the paradoxical predisposition to both bleeding and thrombotic perioperative complications.
Conclusions
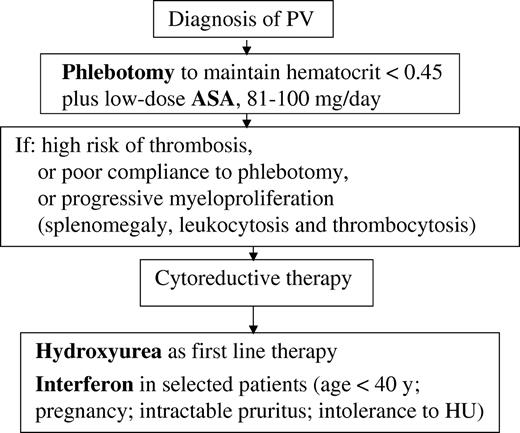
A flow chart summarizing current recommendations for management of patients with PV is shown in Figure 1. These recommendations are based on a limited number of RCTs and large prospective studies, mainly performed by multicenter groups. Clearly, many important clinical questions remain unanswered. There is an urgent need for collaborative networks of basic scientists and clinical investigators, such as the MPD Consortium in the United States and Europe and the LeukemiaNet in Europe, to conduct rigorous studies on large numbers of PV patients well-characterized from a molecular point of view. This need is further emphasized by the recent development of JAK2-targeted drugs, which are expected to represent a major breakthrough for the treatment of PV in the near future.
Flow chart of recommended treatment for patients with polycythemia vera. ASA indicates aspirin.
Flow chart of recommended treatment for patients with polycythemia vera. ASA indicates aspirin.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Guido Finazzi, Department of Hematology, Ospedali Riuniti di Bergamo, Largo Barozzi 1, 24128, Bergamo, Italy; e-mail address: gfinazzi@ospedaliriuniti.bergamo.it.